A 15-week gestation female fetus was delivered for unexplained intrauterine fetal death. The fetus weighed 125g and had a crown heel length of 17cm. Clinical maternal history was unremarkable, with a regular course of gestation until then. At autopsy, no somatic and/or visceral malformations were disclosed. All thoracic and abdominal organs showed initial autolytic changes, the liver was increased in volume, soft tissues appeared edematous and brain was almost completely autolytic.
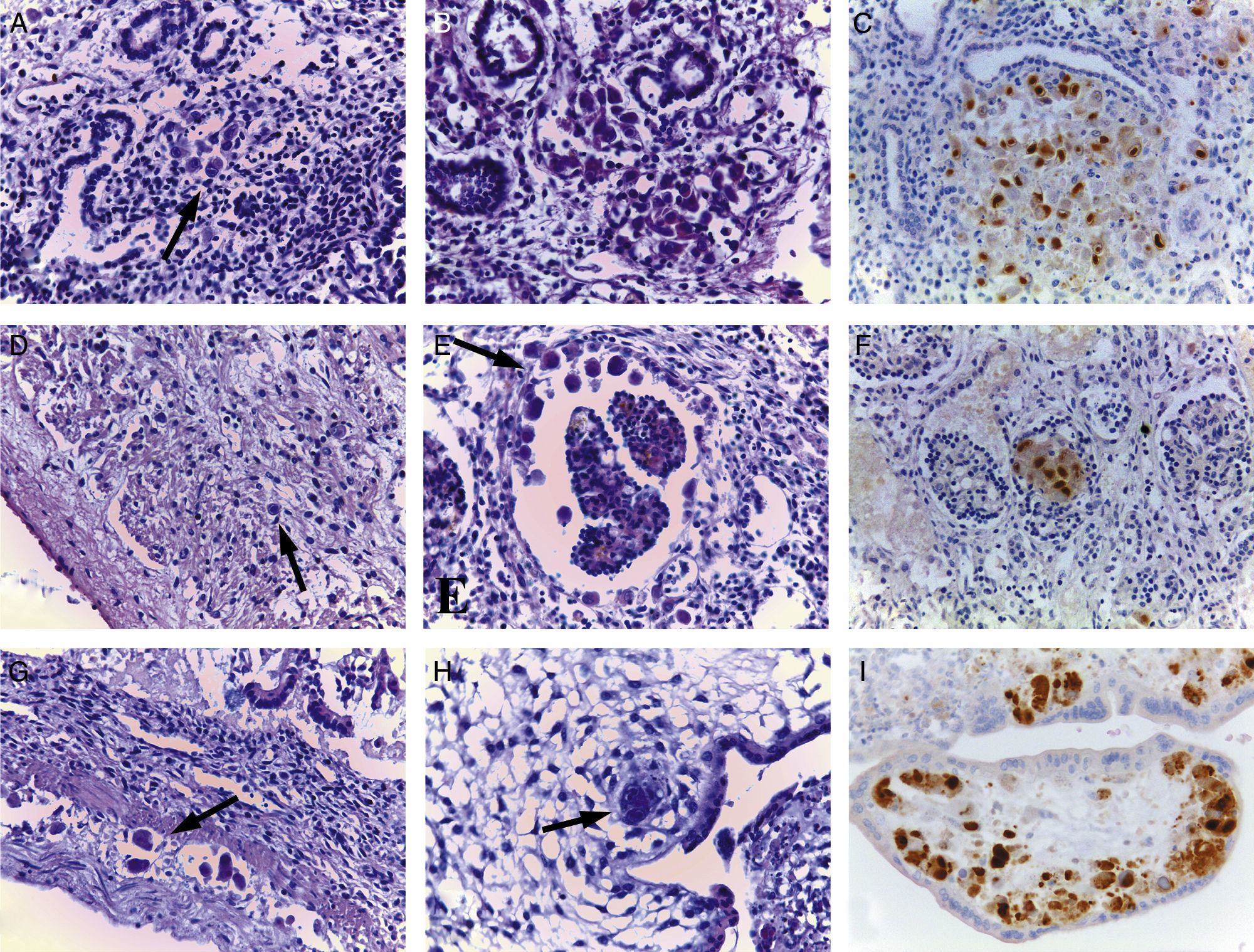
Histology showed several voluminous eosinophilic intranuclear inclusions of probable viral nature in endothelial cells, histiocytes in lung parenchyma (Fig. 1A and B), in myocardiocytes (Fig. 1D), in renal glomeruli (Fig. 1E), small bowel wall (Fig. 1G), and placental chorionic villi (Fig. 1H). The same intranuclear inclusions were also found in adrenal glands, uterus, and in autolytic brain tissue, where assessable. A disseminated fetal cytomegalovirus (CMV) infection was suspected. A positive anti-CMV immunoreaction performed on several tissue sections (Fig. 1C, F, and I) represented the definitive diagnostic tool.
Histology showed several voluminous intranuclear inclusions consistent with CMV infection in endothelial cells and histocytes in lung parenchyma (A–B, arrow, hematoxylin–eosin, 40×), in some myocardiocytes (B, arrow, hematoxylin–eosin, original magnification 40×), in renal glomeruli (E, arrow, hematoxylin–eosin, original magnification 40×), small bowel wall (G, arrow, hematoxylin–eosin, original magnification 40×) and placental chorionic villi (H, arrow, hematoxylin–eosin, original magnification 40×). A positive anti-CMV immunoreaction in lung, renal parenchyma, and placental tissue (C, F, I, original magnification 40×) confirmed the diagnosis of disseminated CMV infection.
Congenital CMV infection results from transplacental transmission of the virus during maternal viremia. The fetus can be infected by either a newly acquired (primary) maternal infection or a recurrent (reactivated) maternal infection. The likelihood of fetal infection and the risk of associated damage and sequelae are higher after a primary infection. Maternal viremia is more likely to occur at primary than recurrent infection.1 After transplacental transmission, the virus spreads through the fetus by hematogenous route. Infection at an earlier gestational age often correlates with a worse outcome and may lead to intrauterine death.2
Cytomegalovirus is a DNA virus of the herpesvirus group which produces an enlargement of the infected cell, and microscopically with hematoxylin–eosin staining, a large 5–15μm sized violaceous to dark red intranuclear inclusion surrounded by a thin clear halo can be seen. At autopsy, diagnosis is most often made histologically by finding the characteristic CMV intranuclear inclusions in the infected organs.3 Immunohistochemistry is useful for detecting CMV, particularly when classic intranuclear inclusions are infrequent or not present.
Conflicts of interestThe author declares no conflicts of interest.