Hepatitis C virus infects over 15 million patients from India and 2.86 million from Brazil. Detection of anti-hepatitis C virus antibodies has limited sensitivity during acute phase: the pre-seroconversion window period. Hepatitis C virus-RNA detection techniques are used to overcome this shortfall, but are costly and unavailable widely in developing countries. Estimation of hepatitis C virus core-antigen, a protein with highly conserved sequence, by enzyme-immunoassays is an economic and simpler alternative to RNA detection. This study was conducted in Delhi, involving 300 acute and chronic liver disease patients, tested for anti-hepatitis C virus 3rd-generation ELISA, hepatitis C virus core-antigen-ELISA and hepatitis C virus-RNA reverse transcription-polymerase chain reaction. Among the acute patients, hepatitis C virus core-antigen assay could identify 13 out of 14 pre-seroconversion window period cases and 6 out of 8 seroconverted cases, with a pre-seroconversion window period sensitivity of 92.9% and specificity of 100%. In hepatitis C virus core-antigen-positive cases, the viral load was in the range of 4900 to 1.46×106IU/mL, whereas in hepatitis C virus core-antigen-negative cases, the range of viral load was 100–4500IU/mL. The cost of the hepatitis C virus core-antigen-ELISA was estimated around 3–4 times lesser than the in-house reverse transcription-polymerase chain reaction and 9–10 times lesser than the United States Food and Drug Administration approved reverse transcription-polymerase chain reaction. With a good sensitivity and specificity in the acute phase of infection, hepatitis C virus core-antigen-ELISA can thus be a useful alternative in the developing nations.
Hepatitis C virus (HCV), a single stranded enveloped RNA virus belonging to the flaviviridae family, is a globally significant pathogen, infecting over 170 million individuals worldwide with about one million new cases being reported annually.1,2 In India, approximately 15 million people are positive for anti-HCV antibodies with reported prevalence of HCV approximately 15–20% in chronic liver diseases (CLD) patients.3 Published data from Brazil showed that around 1.5% of the Brazilian population is anti-HCV positive,4 compounding it to the current population, the HCV infection burden can be estimated to be around 2.86 million. Chronic hepatitis C contributes to approximately 25–40% of all CLD and is the leading cause of liver transplantation worldwide.2 Fewer than 15–25% of cases of acute HCV infections result in the development of jaundice and therefore, the majority of cases are subclinical. But the rate of chronicity following acute HCV infection is pretty high (85%) compared to that of acute hepatitis B virus (HBV) infection (1%).1,2 After infection with HCV, HCV RNA becomes detectable in the serum within days to eight weeks. It is usually present in the blood before the development of jaundice, but the titer of the viral RNA may fluctuate greatly, and some patients may be intermittently negative for the HCV RNA. The minimal interval following a suspected exposure after which a persistently negative HCV polymerase chain reaction (PCR) test rules out infection has not been definitely established.1,2 Approximately one half of patients with symptomatic acute infection have detectable antibodies to HCV detected by ELISA when they first present for care. However, the development of HCV antibodies may be delayed in patients who have subclinical infection. A positive anti-HCV ELISA does not distinguish between those who cleared the infection and those who are chronically infected.2 The possibility of getting false-positive or false-negative results is the drawback of this method. The screening of HCV infection cannot rely solely on anti-HCV ELISA in cases of acute hepatitis C, diagnosis of HCV after occupational exposure, in babies born to HCV infected mothers, in immunocompromised patients and individuals on immunosuppressive therapy, thus warranting the use of other supplemental assay.5 Thus, to overcome these shortfalls of antibody screening for HCV, other supplementary tests are essential,5 of which the molecular biology based techniques to detect HCV RNA are widely used in clinical practice.6 Detection of HCV RNA by nucleic acid amplification techniques (NAT) is expensive, time consuming, requires technical expertise and dedicated laboratory area. These reasons restrict the availability or wide scale usage of HCV RNA detection in many laboratories of developing countries.7,8
HCV core protein is a structural protein and its sequence is highly conserved among all HCV genotypes and quasispecies.9 Detection of HCV core antigens (HCVcAg) for the diagnosis of HCV infection, particularly in the pre-seroconversion window period (PSWP), can be accomplished by several assays that are available for research or commercial purposes, using serum, plasma or whole blood samples.9,10 Ortho Clinical Diagnostic is the most common provider worldwide, with its qualitative screening HCVcAg ELISA and quantitative Ortho trak-c ELISA (Ortho/J&J). There are at least two widely available commercial assays which detect antigen and antibody simultaneously, known as Monolisa Ultra Ag/Ab assay (Marnes-la-Coquette, France) and Murex Ag/Ab combination assay (Abbott Murex, Abbott Murex, Abbott Park, IL) aiming to narrow the window period for positive diagnosis.11
Extensive review reports on the functioning of Murex Ag/Ab combination assay, the Monolisa Ultra Ag/Ab assay and the Ortho HCVcAg assay are available from The Health Protection Agency (HPA), an independent UK organization, set up by the UK government in 2003 for quality control of various drugs and clinical assay techniques.12 The HPA reports have shown that the Ortho HCVcAg assay is the most sensitive kit available in terms of “timing analysis” on the commercial seroconversion panels, when compared to nine other enzyme immuno assays including the Murex Ag/Ab combination assay and the Monolisa Ultra Ag/Ab assay. It detected seroconversion on an average 3.5 days earlier than the Murex Ag/Ab combination assay, 5.5 days earlier than the Monolisa Ultra Ag/Ab assay and 17.6 days earlier than the most sensitive antibody-only EIA, i.e. Vitros ECi anti HCV assay (Ortho/J&J). However, the HPA report had also stated that the antigen-only kits viz. Ortho HCVcAg will usually detect positive specimens early in seroconversion but then may become negative due to suppression of circulating antigen level by the antibody response. Antigen degradation on long term storage of specimens were also conjectured.12
Overall, antigen testing has shown good specificity but currently inadequate sensitivity in the setting of HCV therapeutic monitoring or defining sustained viral response (SVR). However, it has started to gain some popularity in some countries (including resource poor countries) where it has been used for early diagnosis of HCV.11,12
The present study was designed to assess whether the HCVcAg test (Ortho/J&J) is a simple, cost-effective test as compared to NAT and could be a good alternative to NAT for the early diagnosis of HCV infection, particularly in the acute phase of the illness and the PSWP, during which the infection can be missed in a substantial number of cases, if anti-HCV Ab testing is employed alone.
The study was conducted in the Department of Microbiology, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi during the period of May 2006 to July 2009. A total of 300 patients comprising 150 non-A/non-E acute liver disease (ALD) cases and 150 non-metabolic CLD cases were included in the study. The diagnosis of liver disease was based on previously reported clinical, biochemical and histological criteria wherever feasible.2,13 ALD cases included in the study were patients showing clinical and/or biochemical jaundice (with an elevated bilirubin level), with/without history of preceding prodromal symptoms, and increased alanine aminotransferase (ALT) levels (at least 3 times more than the upper limit of normal value) reported at least twice at an interval of one week without any history of previous liver disease. Cases with detectable anti-hepatitis A immunoglobulin M antibody (anti-HAV IgM) and anti-hepatitis E antibody (anti-HEV Ab), previous history of jaundice, suspected and/or diagnosed surgical causes and established metabolic and/or genetic liver diseases were excluded. CLD patients were fresh first contact cases presenting to our hospital and were selected on the basis of clinical and histopathological criteria described by Bianchi et al.13 All CLD patients had continuous higher transaminases level (at least thrice the normal value) for a period of more than six months and histologic evidence of chronic hepatitis on liver biopsy at the beginning of follow-up.2,13 Cases with diagnosed metabolic or genetic liver diseases were excluded from the study. Hepatitis B surface antigen (HBsAg) positive cases were not excluded, due to sharing of common risk factors for infection and wide report of co-infections. A sample with 5mL of blood was collected aseptically from each study subject. Detailed clinical history and clinical examination, including risk factors, was undertaken according to a predesigned protocol. Informed consent was obtained from each patient, and the protocol for the study was approved by the ethical committee and internal review board of the institute. All serum samples were stored at −70°C until tested.
Anti-HCV antibody ELISA: a third generation ELISA Kit, HCV Microlisa (J. Mitra & Co., New Delhi, India) was used to screen the serum samples for the presence of anti-HCV antibodies. The test was performed as per manufacturer's instruction manual.
Detection of HCVcAg: all samples were screened for the presence of HCVcAg by using the HCVcAg qualitative ELISA kit (Ortho Diagnostics/J&J, New Jersey, USA) according to the manufacturer's instructions.
Detection of HCV RNA by reverse transcription-polymerase chain reaction (RT-PCR): viral RNA was extracted from all serum samples using the High Pure Viral RNA Isolation Kit (Roche Diagnostics GmbH, Mannheim, Germany) as per the manufacturer's instructions. The extracted RNA was stored at −70°C until tested.
Qualitative detection of HCV RNA: cDNA was transcribed using specific outer antisense primer (5′-ATGTACCCCATG AG/TA/GTCGGC-3′) from 5′ non-core region (NCR)–core region.14 Reverse transcription was carried out at 42°C for 1h followed by direct PCR in a reaction mixture containing PCR buffer (10×), 2.5mmol/L MgCl2, 10mmol/L dNTPs, 0.75U Taq DNA polymerase (MBI Fermentas, Vilnius, Lithuania) and 20pmol of outer sense and antisense primers (5′-ATGTACCCCATGAG/TA/GTCGGC-3′ and 5′-ACTGCCTGATAGGGTGCTTGCGAG-3′) for 5′ NCR–core region, in a total reaction volume of 25μL. Nested PCR was performed in the reaction mixture containing PCR master mix (2×) and 20pmol inner sense and antisense primers (5′-AGGTCTCGTAGACCGTGCATCATG-3′ and 5′-CAC/TGTA/GAGGGTATCGATGAC-3′) in a total reaction volume of 25μL. The first and second round of PCR comprised 35 cycles at the following conditions: 94°C (denaturation), 55°C (annealing), 72°C (elongation), each for 60s, with final extension at 72°C for 7min. The amplified PCR products were electrophoresed in ethidium bromide–stained 2% agarose gel and visualized in a Gel-Doc System (Alpha Innotech, San Leandro, CA) for identifying desired 405bp fragment using 100bp digested molecular weight marker. Positive and negative controls were also included.14
Quantitative measurement of HCV load: quantitative detection of HCV RNA by real-time PCR was performed in all HCV RNA positive samples using the Roche Light Cycler Taqman Master Kit on Roche Light Cycler 2.0 Real-Time PCR System (Roche Diagnostics GmbH, Mannheim, Germany). Each specimen was analyzed in duplicate and the mean value reported as the HCV RNA level in the serum. A known quantity of internal quality control serum was included in each preparation of RT-PCR. The cycle conditions of RT-PCR include 95°C for 10min, followed by a further 40 cycles at 95°C for 10s, 58°C for 15s and 72°C for 10s.14,16
Standard statistical methods and SPSS software version 18.0 were used to calculate sensitivity, specificity, positive and negative predictive values. The agreement between HCVcAg and HCV RNA for the detection of HCV infection was analyzed by kappa test. Two-sided p-value ≤0.05 was considered statistically significant.
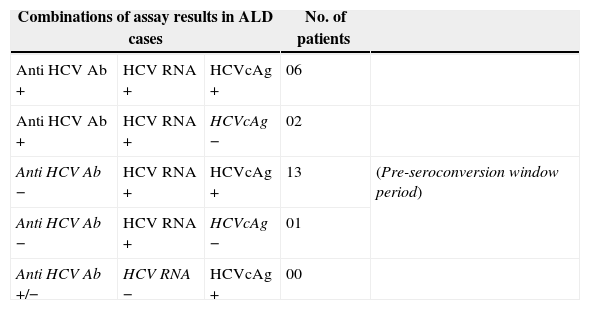
Among the 150 non-A/non-E ALD cases, anti-HCV antibody was detected in eight cases (5.33%). While 22 cases (14.67%) were positive for HCV RNA by RT-PCR and 19 cases (12.66%) were positive for HCV core antigen by HCVcAg assay. None of these 22 HCV RNA positive cases had HBV co-infection. All eight anti-HCV positive cases were positive for HCV RNA and six were positive for HCVcAg. The 14 additional RT-PCR positive cases were presumably in the PSWP (14 out of total 22 PCR positive cases; 63.6%). As the HCV RNA assay is considered gold standard for the ALD cases, among the 142 anti-HCV Ab negative cases (probable pre-seroconversion cases), true HCV infections were present in 14. HCVcAg assay could successfully detect 13 out of these 14 pre-seroconversion cases (92.9%) (Table 1). The single case of ALD, which was undetectable by HCVcAg but detected by RT-PCR had a serum HCV RNA load of 1200IU/mL. The two cases that were anti-HCV Ab positive but HCVcAg negative, had serum HCV RNA levels of 280 and 1350IU/mL, respectively. The sensitivity of HCVcAg assay was 92.86% when compared to HCV RNA in anti-HCV Ab negative cases, and the specificity was 100%. The positive and negative predictive values were 100% and 99.22% respectively. When all the 150 ALD cases were considered, the sensitivity of the HCVcAg assay comes down to 86.36%, probably reflecting undetectable antigen levels in some ALD cases due to high circulating antibody titers (see discussion below). However the specificity and positive predictive value still remains high at 100%.
Results of different assays and their combinations in the cases of non-A/non-E acute liver disease cases.
| Combinations of assay results in ALD cases | No. of patients | |||
|---|---|---|---|---|
| Anti HCV Ab + | HCV RNA + | HCVcAg + | 06 | |
| Anti HCV Ab + | HCV RNA + | HCVcAg − | 02 | |
| Anti HCV Ab − | HCV RNA + | HCVcAg + | 13 | (Pre-seroconversion window period) |
| Anti HCV Ab − | HCV RNA + | HCVcAg − | 01 | |
| Anti HCV Ab +/− | HCV RNA − | HCVcAg + | 00 | |
ALD, acute liver disease; HCV, hepatitis C virus; HCVcAg, HCV core antigens.
Out of the 150 cases of CLD without any diagnosed genetic or metabolic causes, anti-HCV Ab was detected in 41 cases (27.33%) by the third generation ELISA kit (J. Mitra & Co., New Delhi, India) used in our study. HCV RNA was detected in 30 cases (20%) and HCVcAg was detected in 28 cases (18.67%). The 11 cases tested positive for anti-HCV Ab that were negative for HCV RNA, were retested for the presence of anti-HCV Ab and were confirmed to be positive. Confirmation by recombinant immunoblot assay (RIBA) or other methods for antibody detection to detect false positivity of the third generation kit was beyond the scope of this study. Among the CLD cases, HCV RNA and HCVcAg both were positive in 27 cases; three cases were positive for HCV RNA and negative for HCVcAg, and one case was positive for HCVcAg, while negative for HCV RNA, on repeated testing.
In this study, HCV viral load (serum HCV RNA level) was successfully determined in all 52 HCV RNA positive patients. The viral load ranged from 100 to 1.46×106IU/mL with a mean of 2.12×105IU/mL (std. deviation 3.27×105, std. error 4.5×104). In 46 patients who were positive for HCVcAg, the viral load was in the range of 4900–1.46×106IU/mL with a mean of 2.4×105IU/mL (std. deviation 3.38×105, std. error 4.98×105). Whereas in the six samples which were negative for HCVcAg, the viral load was in the range of 100–4500IU/mL with a mean of 1022IU/mL (std. deviation 1711, std. error 698).
The cost per unit tested, were estimated for all the assays and expressed in US dollars (USD), Brazilian Real (BRL) and Indian Rupees (INR). The average cost per sample for HCV Microlisa (J. Mitra & Co.) was 0.85–1 USD (1.7–2 BRL, 47–55 INR). The estimated cost per sample for the HCVcAg assay (Ortho/J&J) was 4.84 USD (9.76 BRL, 267 INR). For the qualitative HCV RNA RT-PCR, it was 13.6 USD (27.16 BRL, 750 INR) and for the in-house quantitative real time PCR, 17.77 USD (35.5 BRL, 980 INR). The costs included only the cost of pack of kits divided by the number of samples (excluding controls), tested per pack. The cost incurred through manpower, establishment and depreciation of instruments were not included for the sake of brevity.
HCV RNA detection by NAT remains gold standard for the early diagnosis during PSWP and for confirmation of active HCV infection.5,6 To reduce the risk of HCV transmission during PSWP, testing of blood products for HCV RNA by NAT is mandatory for European blood banks according to the guidelines of the European Medicinal Evaluation Agency since 1999.7 Detection of HCV RNA by PCR, or derivative methods such as transcript-mediated amplification (TMA), permits the identification of acutely infected donors before their seroconversion for antibody to HCV, who would have been missed by conventional serological tests. High costs, time consumption, requirement of sophisticated equipment and skilled manpower have turned it not to be frequently used in the developing countries of Africa, Asia and Latin America.15 Therefore, during past decades, researchers have put enormous effort to develop HCVcAg ELISA, an otherwise economic and easy to perform assay, as a potential alternative to NAT.6 Our study was intended to evaluate the clinical utility of HCVcAg ELISA in early diagnosis of HCV infection. In India the prevalence of hepatitis C has ranged from 10.8% to as high as 48.5% depending upon the group of patient under observation.15 In this study, the prevalence of HCV ranged from 15.67% to 17.33% depending upon the test used for the detection of infection, among the non-A/non-E ALD cases and non-metabolic CLD cases. The exclusion of enterically transmitted acute viral hepatitis (A and E) and the metabolic and genetic causes of CLD might have increased the prevalence rate in our study. Zhang et al. reported that HCVcAg ELISA is able to identify most of the anti-HCV negative, HCV RNA positive (PSWP) blood donation and reduced the length of undetectable time span.15 In our present study, among the cases of ALD, HCV RNA was detected in 22 cases. HCVcAg was negative in only three cases, where HCV RNA was positive. Out of these three cases, one was in the pre-seroconversion window, and two were positive for anti-HCV Ab. The single case of ALD in the pre-seroconversion window which had undetectable HCVcAg but detectable RT-PCR had a serum HCV RNA load of 1200IU/mL, which was way below our estimated lower limit of detection for the assay (4900IU/mL). The remaining two cases also had lower serum HCV RNA levels (280 and 1350IU/mL respectively) in addition to the presence of high titers of anti-HCV antibodies, which has the ability to neutralize core antigens to below detectable range, as described in earlier reports.12 Only eight cases of ALD were positive for anti-HCV Ab among the 22 cases detected by HCV RNA, leaving 14 cases in the pre-seroconversion window. HCVcAg assay had otherwise successfully detected 13 out of those 14 HCV infected cases. Similar findings have been reported in earlier studies which show the presence of HCV infection by using HCVcAg ELISA during PSWP.9 In this study, the sensitivity, specificity, PPV, NPV of the HCVcAg assay to detect HCV infection, compared to RT-PCR in cases of ALD were 86.36%, 100%, 100% and 97.71% respectively. Almost similar sensitivity was reported by Netski et al. (87%) and Park et al. (90.2%).17,18 In our study, HCVcAg assay demonstrated a specificity of 100% in ALD cases, which is comparable to that reported by Park et al. (100%) and Meidouge et al. (99.2%).10,18 In the present study, viral load was in the range of 100–4500IU/mL in the six HCV RNA positive HCVcAg negative subjects. But, five of the six samples were also positive for anti-HCV Ab, thus leaving a room for chance of the antibodies neutralizing the circulating core antigens to below the detectable level. This is in coherence to the findings of the HPA, UK, where the HCVcAg assay (Ortho/J&J) was reported often to be initially positive, but turn negative as time progresses, even in cases with active HCV replication.12 The sample with the lowest serum level of HCV RNA, which was tested positive for HCVcAg (4900IU/mL) may be accepted as the lower limit of range for analytical sensitivity for HCVcAg assay, from our study. This finding is in agreement with other studies which also recognize the to some extent low sensitivity of HCVcAg assay for detection of HCV infection in low viral load samples.6,17
We found 11 cases of CLD to be positive for anti-HCV Ab, but negative either for HCV RNA or HCVcAg. These cases had biochemical and histological features of CLD. The probable explanations may be false positivity (which seems very less likely, due to the usage of third generation ELISA kit), cleared out infection or persistence of HCV in the liver, otherwise undetected in the serum by HCV RNA PCR or HCVcAg ELISA.
Currently, India has a population of 1210.2 million with a total expenditure on health at purchasing power parity (PPP) per capita of 122 International Dollars (Int. $), which totals to a mere 4.2% of the country's gross domestic product (GDP), ranking 145 among the 194 enlisted countries in the World Health Statistics 2011.19 The blood transfusion system in India is a decentralized, fragmented, and hospital-based system. There are approximately 1800 blood banks in the country, out of which, 45% are governmental, 12% voluntary, 20% private, and 23% commercial. About 3.5million units are collected annually.20 At present, the country does not have a uniformly accepted policy to screen the blood donors for the possible carriage of HCV infection during the PSWP. Though NAT based diagnosis of HCV infections are practiced in certain specialized private blood banks and laboratories, the practice is not widespread due to the obvious reason of cost.20 Brazil, with a population of 190.8 million, has some 6400 hospitals, 620 blood collection sites, and the collection and processing of 4 million units of blood donated per year.20 Spending some 8.4% of GDP, with an average expenditure of 875 Int. $ at PPP per capita on health, Brazil ranks 65th in the WHO list.19 NAT testing had been introduced only in seven blood transfusion services (approximately 100,000units/year total) till 2003,20 and the country also does not seem to have a uniform policy to detect HCV infection during the pre-seroconversion window on a routine basis among the blood donors or ALD patients presenting to the public hospitals. NAT based screening for all blood donors has been introduced in developed countries like United Kingdom and USA at the beginning of this century. But the huge cost to benefit ratio incurred by it on the public exchequer was highly criticized by Simmond et al. in a highly cited commentary published in The Lancet.7 More economic alternatives like the present test used in our study, the Ortho HCVcAg assay was proposed by Diment and Calmann,8 in response to the commentary, citing its successful usage in public health sectors of many European countries. It may have vital significance for the laboratories of developing countries, with a limited resources setup due to its competing cost of 4.84 USD (9.76 BRL, 267 INR) per test, compared to 13.6 USD (27.16 BRL, 750 INR) for the in-house qualitative RT-PCR based HCV RNA detection assay, 17.7 USD (35.5 BRL, 980 INR) for the in-house quantitative real time PCR and 40.98 USD (81.89 BRL, 2261 INR) per unit sample for the United States Food and Drug Administration (FDA) approved COBAS AmpliPrep/COBAS TaqMan HCV assay RT-PCR kit.
Thus, to summarize on the basis of extensive review of literature, we hypothesized that the HCVcAg test may be simple and cost-effective as compared to NAT and that it could be a good alternative to NAT for the early diagnosis of HCV infection, particularly in the acute phase of the illness and the PSWP, during which the infection can be missed in a substantial number of cases, if anti-HCV Ab testing is employed alone. Our study lived up to our assumption to suggest that, the HCV core antigen based ELISA can be used for screening patients presenting with signs and symptoms of acute hepatitis, or in cases of screening for blood donors, in addition to antibody testing, as an alternative to the molecular techniques, where the NAT based tests are not feasible to apply in a mass scale due to economic or technical handicap.
Conflicts of interestThe authors declare to have no conflict of interest.
The authors thank University Grant Commission (UGC), New Delhi, India for the grants provided for the study, Mrs. Sweta Sinha, for her assistance during ELISA and Dr. P. Kar, Director Professor, Department of Medicine, Maulana Azad Medical College, New Delhi, India for his support during the study.