Treatment of orthopedic infections usually requires prolonged antimicrobial therapy, ranging from 14 days up to 6 months. Nowadays, rising levels of antimicrobial resistance demands parenteral therapy for many patients. Outpatient parenteral antimicrobial therapy (OPAT) is a modality that allows treatment out of hospital in these situations. In Brazil, where a public universal healthcare system allows full coverage for all citizens, implantation and dissemination of OPAT programs would be beneficial for patients and for the system, because it would allow a better allocation of health resources. The Instituto de Ortopedia e Traumatologia do Hospital das Clínicas da Faculdade de Medicina da USP (IOT) started, in July 2013, a partnership with municipal health authorities in Sao Paulo, Brazil, in order to initiate an OPAT program in which patients discharged from that hospital would be able to continue antimicrobial therapy at primary care facilities. When necessary, patients could also receive their therapy at the day-hospital located at IOT. Primary care nursing and physician staff were trained about antimicrobial infusion and peripherally inserted central catheter manipulation. An OPAT specific antimicrobial protocol was designed and a special reference and counter-reference organized. As a result, 450 primary healthcare professionals were trained. In the first year of this program, 116 patients were discharged for OPAT. Chronic and acute osteomyelitis were most frequent diagnosis. Teicoplanin, ertapenem and tigecycline were the most used drugs. Duration of treatment varied from 10 to 180 days (average 101, median 42). Total sum of days in OPAT regimen was 11,698. Only 3 patients presented adverse effects. Partnership between services of different levels of complexity allowed implantation of a safe and effective public healthcare OPAT program for treatment of orthopedic infections. This program can serve as a model for developing similar strategies in other regions of Brazil and Latin America.
Due to special features related to blood supply and local immunological mechanisms related to defense against infection, treatment of orthopedic infections (including bone, joint, and soft tissue infections) usually requires prolonged antimicrobial therapy, ranging from 14 days up to six months in cases of arthroplasty-related chronic osteomyelitis.1–4 In this setting of long-lasting therapy, rising levels of antimicrobial resistance demands full parenteral therapy for many patients. Outpatient parenteral antimicrobial therapy (OPAT) is a modality that allows for treating these cases outside the hospital. OPAT has been widely used in some countries, with consolidated programs and specific guidelines to help OPAT services to provide quality patient care and to minimize clinical risk.5–7 In Latin America, however, no OPAT programs were implanted and described until now.
In Brazil, a public universal healthcare system provides full coverage for all citizens. In this model of healthcare, it is believed that implantation and dissemination of OPAT programs would be beneficial for the patients and for the system. It would allow for better allocation of hospital resources and offer a highly clinically efficacious, cost-effective, and safe alternative to inpatient care where parenteral therapy is deemed necessary. Brazilian healthcare organization provides ranking of services into primary, secondary, and tertiary levels according to the degree of complexity. Generally, tertiary and secondary-care facilities are under federal or state administration. Primary care facilities, otherwise, are under municipal regulation. Reference and counter-reference protocols should integrate the different levels of healthcare services.8 Establishing an OPAT program in this healthcare system would require these protocols to be implemented and published, in order to assure safety and efficacy for outpatient therapy.
ObjectiveTo describe the implementation process and the preliminary results of a public healthcare OPAT program for treating orthopedic infections in Sao Paulo, Brazil.
MethodsThe Instituto de Ortopedia e Traumatologia do Hospital das Clínicas da Faculdade de Medicina da USP (IOT) is a tertiary hospital linked to the University of São Paulo and dedicated to care for high-complexity orthopedic patients in São Paulo, Brazil. In July 2013, this hospital started a partnership with local municipal health authorities in order to initiate an OPAT program in which patients discharged from that hospital would be able to continue antimicrobial therapy at primary care facilities located near their homes. When this was not possible, patients could also receive therapy at the day-hospital located at IOT.
Before starting this OPAT program, primary care nurses staff were trained by IOT professionals about antimicrobial infusion techniques and manipulation of central lines. Peripherally inserted central catheter (PICC) was considered as the first choice of central line in this protocol, Hickman lines (HL) were used when PICC insertion was not possible. Hands-on workshops were designed especially for manipulation of both devices, in order to familiarize the professionals with them. Dressing changes were performed once a week for PICC and HL. PICC lines were flushed with 10mL saline solution immediately before and after antimicrobial infusion. HL were also flushed with 3mL of heparin solution (300UI/mL) after infusion, and this solution was aspirated before the next antimicrobial infusion. Primary care physicians were trained, also by IOT staff, on clinical monitoring of patients during OPAT.
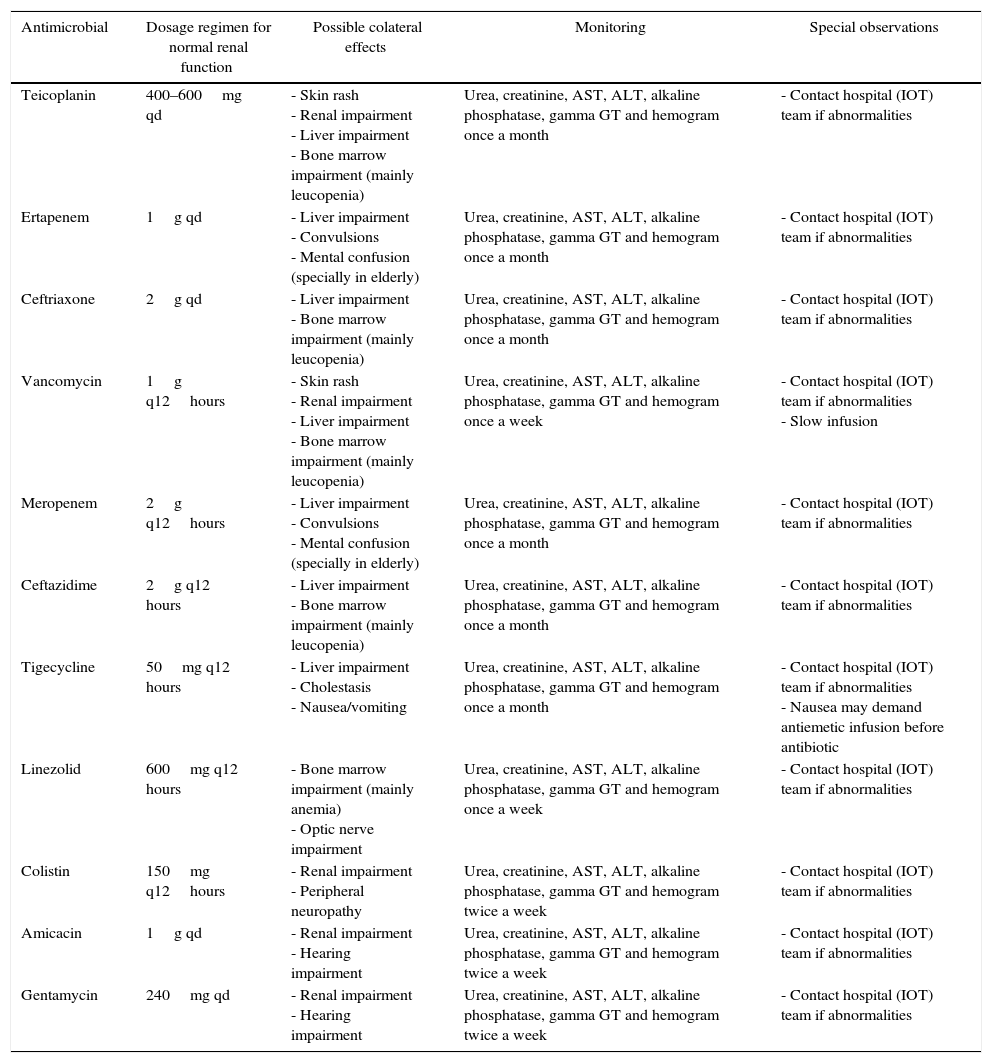
An OPAT specific antimicrobial protocol was designed in order to prioritize infusions qd or bid during the day and with specific instructions when necessary (Table 1). Also, a special reference and counter-reference pathway was organized specially to this program, in order to assure rapid referral to IOT in case of adverse events related to antimicrobial infusion. This pathway also included previous communication to primary-care or day-hospital staff before patient discharge to OPAT, as well as a written detailed planning about patient care outside the hospital. Patients and their caregivers received information about adequate CL care and the importance of adhering to the protocol.9
Specific antimicrobial protocol for outpatient parenteral antimicrobial therapy.
| Antimicrobial | Dosage regimen for normal renal function | Possible colateral effects | Monitoring | Special observations |
|---|---|---|---|---|
| Teicoplanin | 400–600mg qd | - Skin rash - Renal impairment - Liver impairment - Bone marrow impairment (mainly leucopenia) | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a month | - Contact hospital (IOT) team if abnormalities |
| Ertapenem | 1g qd | - Liver impairment - Convulsions - Mental confusion (specially in elderly) | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a month | - Contact hospital (IOT) team if abnormalities |
| Ceftriaxone | 2g qd | - Liver impairment - Bone marrow impairment (mainly leucopenia) | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a month | - Contact hospital (IOT) team if abnormalities |
| Vancomycin | 1g q12hours | - Skin rash - Renal impairment - Liver impairment - Bone marrow impairment (mainly leucopenia) | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a week | - Contact hospital (IOT) team if abnormalities - Slow infusion |
| Meropenem | 2g q12hours | - Liver impairment - Convulsions - Mental confusion (specially in elderly) | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a month | - Contact hospital (IOT) team if abnormalities |
| Ceftazidime | 2g q12 hours | - Liver impairment - Bone marrow impairment (mainly leucopenia) | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a month | - Contact hospital (IOT) team if abnormalities |
| Tigecycline | 50mg q12 hours | - Liver impairment - Cholestasis - Nausea/vomiting | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a month | - Contact hospital (IOT) team if abnormalities - Nausea may demand antiemetic infusion before antibiotic |
| Linezolid | 600mg q12 hours | - Bone marrow impairment (mainly anemia) - Optic nerve impairment | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram once a week | - Contact hospital (IOT) team if abnormalities |
| Colistin | 150mg q12hours | - Renal impairment - Peripheral neuropathy | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram twice a week | - Contact hospital (IOT) team if abnormalities |
| Amicacin | 1g qd | - Renal impairment - Hearing impairment | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram twice a week | - Contact hospital (IOT) team if abnormalities |
| Gentamycin | 240mg qd | - Renal impairment - Hearing impairment | Urea, creatinine, AST, ALT, alkaline phosphatase, gamma GT and hemogram twice a week | - Contact hospital (IOT) team if abnormalities |
The main inclusion criterion for this protocol was indication for prolonged parenteral antimicrobial therapy, based on results of culture and antimicrobial susceptibility tests. In addition, patients were to be clinically stable, regarding both the infectious condition and possible associated comorbidities. Exclusion criteria were inability to understand the risks of intravenous therapy and appropriate care of CL, as well as the lack of adequate transport to where antimicrobials would be infused (primary care facility or day-hospital). Patients with history of active drug addiction or alcoholism were also excluded from the protocol because of the risk of improper manipulation of the CL.
In November 2013, after these initial steps, this OPAT program was started.
ResultsAs a result of this partnership, 450 primary healthcare professionals were trained, including nurses and physicians. In the first year of this program, until November 2014, 116 patients were discharged for continuing antimicrobial therapy in outpatient setting. There was a predominance of male patients (72%) and the average age of the group was 39.3 years (variation from 8 to 76 years, median 38 years). A total of 82 patients (70%) received therapy at primary care facilities and 34 (30%) at the day-hospital located at IOT. The vast majority of the group involved in this protocol, 114 patients (98.3%), used PICC lines for antimicrobial infusion, only two patients (1.72%) used HL.
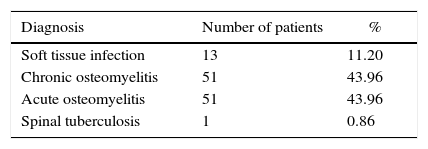
Chronic and acute osteomyelitis were the most frequent diagnosis, 51 patients (43.96%) of each diagnosis. Table 2 shows the patient distribution according to diagnosis; 98 patients (84.5%) received only one antimicrobial and 18 patients (15.5%) were treated with a combination of two antimicrobials. One patient, with spinal tuberculosis and intolerance to ethambutol needed therapy with streptomycin, a drug that was not initially included in OPAT protocol. It was necessary to include intravenous linezolid in this protocol because of the financial difficulties to access the oral presentation of this drug at public healthcare setting in Brazil.
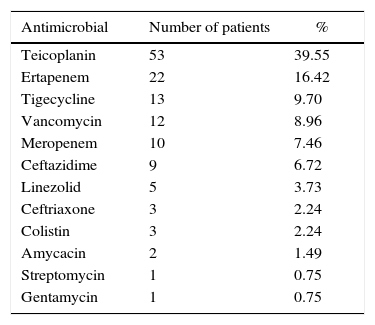
Teicoplanin (40%), ertapenem (16%), and tigecycline (10%) were the most frequently used antimicrobials, as shown in Table 3. The duration of treatment varied from 10 to 180 days (average 101 days, median 42 days). The total sum of days in OPAT regimen was 11,698.
Antimicrobials used for treating orthopedic infections in outpatient parenteral antimicrobial therapy.
| Antimicrobial | Number of patients | % |
|---|---|---|
| Teicoplanin | 53 | 39.55 |
| Ertapenem | 22 | 16.42 |
| Tigecycline | 13 | 9.70 |
| Vancomycin | 12 | 8.96 |
| Meropenem | 10 | 7.46 |
| Ceftazidime | 9 | 6.72 |
| Linezolid | 5 | 3.73 |
| Ceftriaxone | 3 | 2.24 |
| Colistin | 3 | 2.24 |
| Amycacin | 2 | 1.49 |
| Streptomycin | 1 | 0.75 |
| Gentamycin | 1 | 0.75 |
Only three patients presented adverse effects during OPAT and required readmission to the hospital. Two patients had signs of infection related to PICC line insertion, without blood stream dissemination, and one patient had liver impairment and cholestasis during therapy. All of them had favorable outcomes after specific measures.
DiscussionOPAT has already demonstrated its suitability, as it leads to faster return home to daily activities and less risk of acquiring healthcare-related infections and other severe complications.10,11 Beyond these direct benefits for the patients eligible for this modality of antimicrobial treatment, OPAT also can indirectly benefit the healthcare system by allowing better allocation of financial resources and in-hospital bed availability. This is of particular importance in countries with universal public healthcare coverage, such as Brazil. Our OPAT protocol for orthopedic infections, including those related to soft tissue or bone and joint, made possible, in one year alone, 11,698 bed-days at the orthopedics ward to be redirected to patients really needing to be hospitalized, such as trauma victims or those requiring elective surgeries.
Only three patients presented adverse effects during this OPAT program, all of them rapidly diagnosed and solved. This finding demonstrates that training of primary care professionals for massive use of PICC lines as infusion devices was effective, as well as the reference and counter reference protocol developed.
This study has some limitations, since it did not assess patients’ satisfaction and quality of life of those on OPAT. In addition, no cost-effectiveness analysis of OPAT was undertaken. Therefore, more comprehensive studies evaluating OPAT in Brazilian and Latin American settings are warranted.
ConclusionThe partnership between medical services of different levels of complexity allowed for the establishment of a safe and effective OPAT program for treating orthopedic infections in public health centers of São Paulo, Brazil. This program can serve as a model for developing similar strategies in other regions of Brazil and Latin America.
Conflicts of interestThe authors declare no conflicts of interest.