Vaccination with tetanus-diphtheria-acellular pertussis (Tdap) has been recommended for healthcare workers (HCWs) by Brazilian Ministry of Health since November 2014.
ObjectiveTo describe the strategies implemented to improve Tdap uptake, cumulative vaccine coverage after each intervention, variables associated to Tdap vaccination, and reasons for non-vaccination among HCWs of the main building of a quaternary hospital attached to the Sao Paulo University Medical School.
MethodsA list of HCWs eligible for pertussis vaccination was generated. From April to December 2015, the following interventions were implemented: note on intern journal reminding the importance of pertussis vaccination; email to the head nurses strengthening vaccine recommendations; lectures on pertussis and Tdap for physicians of Obstetrics and Neonatology Clinics; on-site vaccination by mobile teams at the Obstetrics, Neonatology, and Anesthesiology Clinics. Vaccine coverage was accessed at the end of each month. Multivariate Poisson regression model with a robust error variance was used to evaluate variables associated with Tdap vaccination. Reasons for non-vaccination were evaluated from January to May 2017 through phone calls for HCWs who had not received Tdap.
ResultsThe study included 456 HCWs. After the interventions, Tdap coverage raised from 2.8% to 41.2%. In the multivariate analysis, occupation (physician), working place (obstetrics or anesthesiology) and influenza vaccination in 2015 were independently associated to Tdap vaccination. The main reason for non-vaccination was unawareness of Tdap recommendations.
ConclusionsTdap uptake among HCWs was low in our hospital. Providing vaccination at convenient places/times for HCW seems to be the most efficient strategy to increase vaccine uptake.
Adult vaccination is difficult to implement. Most countries have low vaccine coverage among adults. Immunization of healthcare workers (HCWs) is challenging, as they usually show low perception of personal risk involved in their professional activities1,2 and hesitate in receiving vaccines. Fear of injections, misconceptions about vaccines efficacy and safety and lack of time are common reasons for non vaccination among HCWs.3
Vaccines recommended for HCWs include influenza, hepatitis B, measles-mumps-rubella, varicella, tetanus-diphtheria and, in some countries, adult tetanus-diphtheria-pertussis acellular vaccine.4
Pertussis is caused by Bordetella pertussis, a Gram-negative bacillus transmitted by aerosol droplets.5,6 It affects people of all ages, but children aged less than one year are most affected.7 During the last decades, pertussis incidence raised globally, in spite of sustained high childhood vaccination coverage.6 Waning immunity after vaccination or infection, reduced effectiveness/duration of protection conferred by acellular pediatric vaccines, increased disease awareness, improved diagnoses and surveillance, and B. pertussis mutations allowing it to escape immunity conferred by vaccines have been proposed to explain pertussis reemergence.5,6 In Brazil, pertussis incidence increased from 0.3/100,000 persons in 2010 to 4/100,000 in 2014, despite high coverage with whole-cell vaccines in children.8 Most cases occurred in infants among whom the incidence rate increased from 18/100,000 in 2010 to 152/100,000 in 2014, and who also had the highest case-fatality rate (4.6% among infants less than two months of age).8
Several Tdap vaccination strategies targeting adults to reduce pertussis among young infants have been proposed, including pregnant women vaccination, the cocooning strategy (vaccinating all newborns contacts), and vaccination of adolescents and adults, including HCWs.5 HCWs are at increased risk of acquiring pertussis through contact with infected patients and waning immunity following childhood vaccination or natural infection.9 Therefore, HCWs could be a source of pertussis nosocomial outbreaks.10 Recommendations on Tdap vaccination for HCWs vary by country. Some countries, such as the United States, Canada, Australia, Netherlands, Germany, and United Kingdom adopted Tdap vaccination for all HCWs, while others, such as Austria, Finland and Norway introduced Tdap only for HCWs who have contact with newborns and infants.11 In Brazil, Tdap was introduced into the Brazilian National Immunization Program (PNI) in November 2014, targeting pregnant women and HCWs who are in contact with newborns.12
The “Instituto Central do Hospital das Clinicas” (ICHC) is the main building of a quaternary teaching hospital attached to the Medical School of Sao Paulo University (FMUSP), which is the largest hospital in Latin America. ICHC has 850 beds. The “Centro de Referência para Imunobiológicos Especiais do Hospital das Clínicas” (CRIE-HC) is the immunization center of the complex and provides free vaccination as recommended by the PNI. In March 2015, four months after Tdap introduction, vaccine coverage among HCWs of the ICHC for whom the vaccine was recommended was very low (2.8%).
This study describes the strategies implemented in 2015 to raise Tdap uptake, the cumulative coverage after each strategy and the variables associated to Tdap vaccination among the HCWs of the ICHC.
MethodsA descriptive observational study was designed. Inclusion criteria: to be a HCW of the ICHC eligible for pertussis vaccination according to PNI recommendations. A list of HCWs with the recommendation was provided by ICHC direction. Exclusion criteria: not registered on the CRIE-HC data system (Imuni®), which had the vaccination history of all service users. If the HCW was not registered on Imuni®, it implies that he/she had never received a vaccine in that service.
To plan the interventions, we used our group experience with seasonal influenza campaigns13 and from published papers on Tdap campaigns.14–16
The following interventions were implemented aiming to raise vaccine coverage:
- •
April 2015: a note on the hospital intern journal, reminding the PNI recommendations on Tdap vaccination, and the importance and safety of pertussis vaccination for HCWs. The intern journal is a monthly printed magazine, also available on line, with news and informs from the hospital to the employees.
- •
July 2015: emails to the head nurses of Obstetrics, Neonatology and Anesthesiology Clinics, strengthening the need of Tdap vaccination.
- •
August 2015: a lecture on pertussis and Tdap immunization for physicians at the clinical rounds of Obstetrics and Neonatology divisions.
- •
October 2015: on-site vaccination by mobile teams at convenient time for the HCWs at the Obstetrics Clinic.
- •
November 2015: on-site vaccination at the Neonatology Clinic.
- •
December 2015: on-site vaccination at the Anesthesiology Clinic.
Access to vaccination was improved through on-site vaccination at the professional’s workplace, at convenient times for the HCWs, by mobile teams carrying coolers stocked with Tdap vaccine, a minimum-maximum thermometer, ice packs, syringes, alcohol hand rub, alcohol wipes, adhesive bandages, disposal containers for needles, and documentation forms. The on-site vaccination was performed in two morning periods at the Obstetrics and Neonatology Clinics and in an evening period at the Anesthesiology Clinic.
Reasons for non-vaccination were evaluated through phone calls (maximum of three attempts for each HCW) from January to May 2017 for those HCWs that had not received Tdap. A standardized questionnaire was applied, asking if the HCW knew the vaccine, if he had received Tdap in another service and, if not, the reason for not being vaccinated. HCWs that did not have a phone number registered on Imuni® could not be evaluated.
The following variables were also retrieved from the Imuni® system: age at vaccination, sex, occupation (physician or multi-professional team) and influenza vaccination in 2015.
Statistical analysisData from the Imuni® system was used for the vaccine coverage analyses. It was calculated by dividing the number of HCWs vaccinated with Tdap by the total number of HCWs with vaccine recommendation and expressed as percentage. Vaccine coverage was accessed at the end of each month from March 2015 to April 2016.
After collecting the variables, a data bank was developed in Microsoft Excel and analyzed in STATA version 13.0 (StataCorp LP, College Station, Texas, USA). To evaluate the variables associated with Tdap vaccination, the Chi-squared test (or Fischer exact test, when appropriate) were used, in the univariate analysis, to calculate the prevalence ratio and their 95% confidence interval (95%CI). Those variables with p < 0.2 were included in a multivariate analysis. Multivariate Poisson regression model with a robust error variance was used. The modeling process was initiated with the variable with the lowest p-value in univariate analysis. The variables were successively added to the model, and only those with p < 0.05 stayed in the final model.
Ethical approvalThis project was approved by the Committee of Ethics in Research of the Hospital das Clinicas (CAPesq n°1.662.341).
ResultsStudy populationAmong the 515 HCWs who were eligible for Tdap immunization according to PNI criteria, it was not possible to evaluate the vaccine status of 59 professionals, because they were not registered on the Imuni® system and they were not found during the strategies implementation. We could not ascertain if these 59 professionals received all vaccines (including Tdap) in another health service or if they were not vaccinated. Therefore, they were excluded from the analyses. Thus, a total of 456 HCWs were included.
The majority of the study population was female (77%), under 35 years-old (50.2%), physicians (50.1%), worked at the Obstetrics Clinic (42.3%), and had not received influenza vaccination in 2015 (56.7%). Thirteen HCWs were nutritionists or physiotherapists. As they were few, for the purpose of the statistical analysis, they were lumped together with the nursing team in the multi-professional team.
There were no differences regarding sex (p = 0.448), age (p = 0.999), occupation (p = 0.383), and place of work (p = 0.847) among the 456 HCWs included and the 59 excluded (Supplementary Appendix).
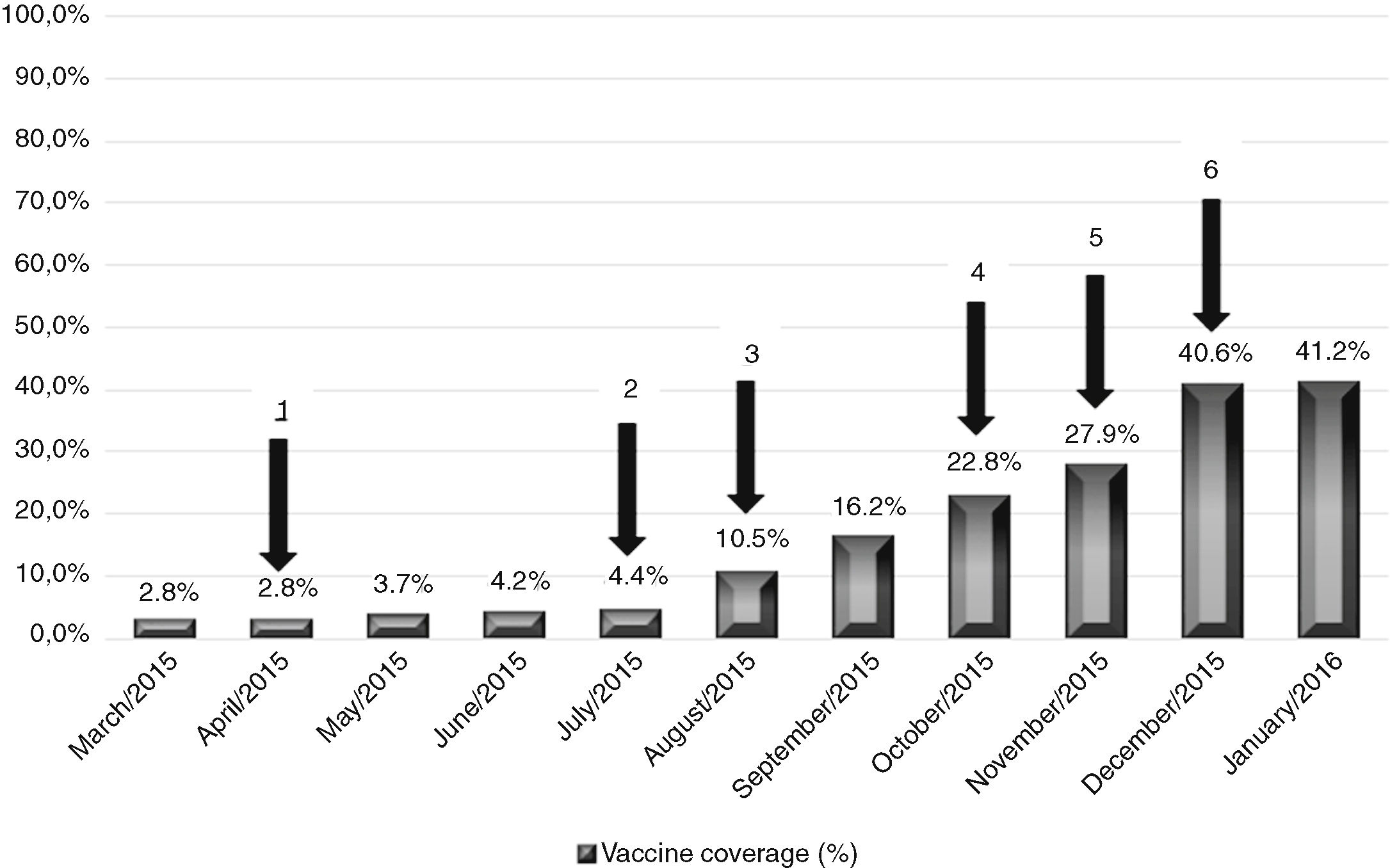
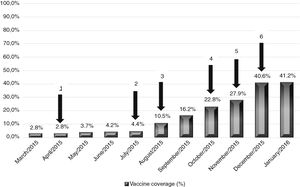
Tdap coverageOn January 2016, nine months after implementing the strategies to increase vaccine coverage, Tdap coverage raised from 2.8% (13/456) to 41.2% (188/456), an increase of 38.3%. Fig. 1 shows the cumulative Tdap vaccine coverage among HCWs at the end of each month and the moment when the strategies were implemented. Spreading information on pertussis and Tdap vaccination (note in internal journal, emails to the teams and lectures to the targeted HCW) raised vaccine coverage in 13.4% (from 2.8% to 16.2%) whereas providing on-site vaccination by mobile teams at convenient times for the HCW increased Tdap coverage in 25% (16.2–41.2%). No other intervention was implemented from December 2015 to March 2016, and the vaccine coverage remained stable (41.2% in April 2016).
Cumulative Tdap vaccine coverage at the end of each month and interventions implemented. Arrows represents the interventions: (1) publication note on our intern journal; (2) email to the nurse team chiefs; (3) lecture on pertussis for physicians; (4) on-site vaccination at the Obstetrics Clinic; (5) on-site vaccination at the Neonatology Clinic; (6) on-site vaccination at the Anesthesiology Clinic. Instituto Central do Hospital das Clínicas (ICHC), São Paulo, Brazil, March 2015 to January 2016.
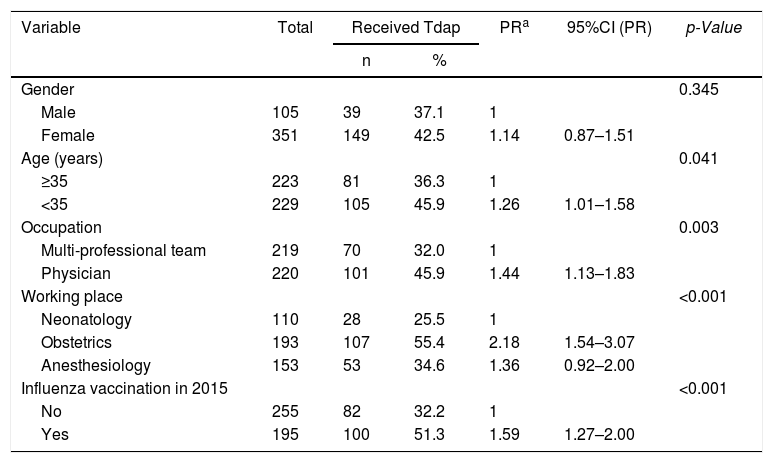
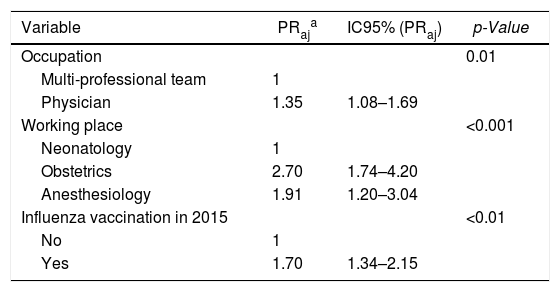
In the univariate analysis (Table 1), higher Tdap coverage was associated with age (<35 years-old), occupation (physician), working place (obstetrics or anesthesiology), and influenza vaccination in 2015. In the multivariate analysis, occupation (physician), working place (obstetrics or anesthesiology), and influenza vaccination in 2015 were independently associated to Tdap vaccination (Table 2).
Variables associated with Tdap vaccination among healthcare workers of a quaternary university hospital in univariate analysis. Instituto Central, Hospital das Clinicas — ICHC, Sao Paulo, Brazil.2015–2016.
| Variable | Total | Received Tdap | PRa | 95%CI (PR) | p-Value | |
|---|---|---|---|---|---|---|
| n | % | |||||
| Gender | 0.345 | |||||
| Male | 105 | 39 | 37.1 | 1 | ||
| Female | 351 | 149 | 42.5 | 1.14 | 0.87–1.51 | |
| Age (years) | 0.041 | |||||
| ≥35 | 223 | 81 | 36.3 | 1 | ||
| <35 | 229 | 105 | 45.9 | 1.26 | 1.01–1.58 | |
| Occupation | 0.003 | |||||
| Multi-professional team | 219 | 70 | 32.0 | 1 | ||
| Physician | 220 | 101 | 45.9 | 1.44 | 1.13–1.83 | |
| Working place | <0.001 | |||||
| Neonatology | 110 | 28 | 25.5 | 1 | ||
| Obstetrics | 193 | 107 | 55.4 | 2.18 | 1.54–3.07 | |
| Anesthesiology | 153 | 53 | 34.6 | 1.36 | 0.92–2.00 | |
| Influenza vaccination in 2015 | <0.001 | |||||
| No | 255 | 82 | 32.2 | 1 | ||
| Yes | 195 | 100 | 51.3 | 1.59 | 1.27–2.00 | |
Variables associated with Tdap vaccination among healthcare workers of a quaternary university hospital in multivariate Poisson regression model. Instituto Central, Hospital das Clinicas — ICHC, Sao Paulo, Brazil.2015–2016.
| Variable | PRaja | IC95% (PRaj) | p-Value |
|---|---|---|---|
| Occupation | 0.01 | ||
| Multi-professional team | 1 | ||
| Physician | 1.35 | 1.08–1.69 | |
| Working place | <0.001 | ||
| Neonatology | 1 | ||
| Obstetrics | 2.70 | 1.74–4.20 | |
| Anesthesiology | 1.91 | 1.20–3.04 | |
| Influenza vaccination in 2015 | <0.01 | ||
| No | 1 | ||
| Yes | 1.70 | 1.34–2.15 |
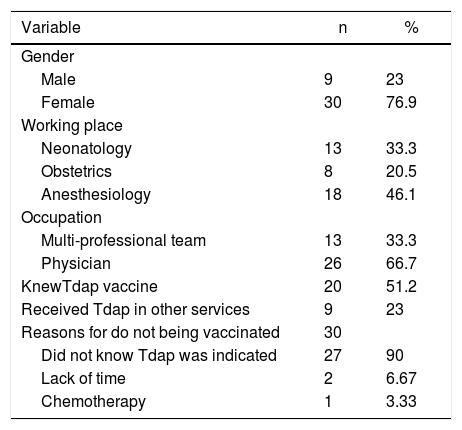
Among the 268 HCWs who had not been vaccinated, 94 did not have a phone number registered on Imuni® system. Therefore, we attempted phone contact with 174 HCWs who had not received Tdap. For eight of then, the recorded phone number was incorrect, and contact was not possible either. Only 39 (22.4%) of the 174 HCWs could ultimately be contacted. Their characteristics and reasons for non-vaccination are shown on Table 3.
Characteristics of 39 healthcare workers of a quaternary university hospital who did not receive Tdap and reasons for non-vaccination. Instituto Central, Hospital das Clinicas — ICHC, Sao Paulo, Brazil, 2015–2016.
| Variable | n | % |
|---|---|---|
| Gender | ||
| Male | 9 | 23 |
| Female | 30 | 76.9 |
| Working place | ||
| Neonatology | 13 | 33.3 |
| Obstetrics | 8 | 20.5 |
| Anesthesiology | 18 | 46.1 |
| Occupation | ||
| Multi-professional team | 13 | 33.3 |
| Physician | 26 | 66.7 |
| KnewTdap vaccine | 20 | 51.2 |
| Received Tdap in other services | 9 | 23 |
| Reasons for do not being vaccinated | 30 | |
| Did not know Tdap was indicated | 27 | 90 |
| Lack of time | 2 | 6.67 |
| Chemotherapy | 1 | 3.33 |
Within these 39 HCWs, 20 (51.2%) reported knowing Tdap vaccine. Eighteen of them (90%) were physicians and two (2%) belonged to the multi-professional team. Nine HCW (45%) works on neonatology, three on obstetrics clinics, and one at anesthesiology.
All nine HCWs that reported having received Tdap vaccine were physicians. Seven received Tdap on a public health service and two at a private health service. One HCW was under chemotherapy and chose not to receive the vaccine, even though it is an inactivated vaccine, without contraindication for immunosuppressed persons.
DiscussionTo our knowledge, this is the first evaluation of Tdap coverage among HCWs in Brazil. Spontaneous adherence to Tdap immunization among HCWs with direct contact with infants was very low at this quaternary university hospital in Sao Paulo. We initiated our interventions with a vaccine coverage of 2.8% and achieved a cumulative coverage of 41.2% in nine months. This incremental of 38.3% in vaccine coverage was attributed to the strategies implemented. Increasing awareness of pertussis illness and the need of Tdap immunization among HCWs helped to increase vaccine uptake, but we believe vaccinating the targeted HCWs at their work place during working hours by mobile teams was critical to increase vaccine coverage quickly. However, the final Tdap coverage among our HCWs is still low and greater and continuous efforts are necessary to impove it.
Few studies analyzed pertussis immunization coverage specifically among HCWs and their results are discrepant. Recently, our group performed a systematic review of Tdap coverage among HCWs.17 Among the 28 studies included in the review, only five reported strategies performed to raise vaccine coverage.14–19
The first one was carried out in a pediatric hospital in Switzerland, where Tdap vaccination program was implemented during one year. The program, like the one developed by us, involved informative messages and lectures. Differently, they scheduled appointments for counseling each HCW. The overall pertussis vaccine coverage was 49%. Among the HCWs that underwent counseling, vaccine coverage raised from 17% to 88%.14
In another evaluation of Tdap vaccination in a paediatric hospital in the United States, the coverage rose from 58% to 90% after 15 months. The authors sent information by email and through the institution intranet, conducted individual interviews with HCWs and established vaccination sites in places of high flow of HCWs.15 In the United Kingdom, one hospital achieved a Tdap coverage rate of 86% and another achieved 95%, three months after implementing informative posters, oral presentations and HCW vaccination at their work sites.16 In the United States, two services have achieved higher pertussis vaccine coverage among HCWs with mandatory vaccination programs.18,19 In Philadelphia, the Geisinger Health System, which employed 15,267 HCWs, had an initial Tdap coverage of 9%, which increased to 97.8%, after one year of mandatory HCWs vaccination.19 The Atlantic Health System also introduced mandatory HCWs vaccination in 2013, reaching a final Tdap coverage of 94.9%.18 In Brazil, HCW vaccination is not mandatory, but vaccination is free of charge for those who fulfill PNI recommendations. Unfortunately, free availability is not enough to guarantee high vaccine uptake.
Two countries have national-based data on Tdap coverage among HCWs.20,21 The National Health Interview Surveillance (NHIS), in the United States, observed that 45.1% HCWs had receive Tdap in 2015.22 In France, among 1431 HCW who self-reported vaccination, higher coverage (63.9%) was found.21 These two studies found significant difference on Tdap coverage among different geographic area of their countries.21,22 In Brazil, data on vaccine coverage among HCW is not routinely available. The country has continental dimensions and great regional socioeconomic, cultural, and health system structure differences. Our results may not be apply to other regions of the country or to other types of services, and more studies of Tdap coverage are necessary.
We observed that being physician, working on obstetrics or anesthesiology departments, and having received influenza vaccine in the same year were independently associated with Tdap vaccination. Others studies also observed association of HCW pertussis immunization with being physician21 and influenza vaccination.9,21 Age under 49 years,9,21 higher education level, having been hospitalized within the past year, having a clinic or health center as the usual place for health care,9 and hepatitis B immunization were all found to be associated to Tdap vaccination in other studies.21
The association between influenza and Tdap immunization could reflect a self-behavior of some HCWs, more used to seek healthcare, including immunization. The final Tdap coverage observed among HCWs with recommendation of Tdap vaccination in our hospital (41.2%) was similar to the influenza vaccine coverage in 2015 (43.3%) among HCWs included in the study, a vaccine that they are more acquainted and which has annual campaigns.
Educational interventions and improved access to vaccination, similar to those adopted for Tdap, were previously implemented to raise influenza vaccine coverage in our hospital, which increased from 6.5% in 2005 to 45% in 2006.13 In the following years, influenza vaccination at the HCW workplace by mobile teams was maintained and the number of HCWs vaccinated was sustained. In 2015, a total of 9,678 (48.5%) HCWs received the influenza vaccine.
Partially, low Tdap coverage could be attributed to lower awareness of the vaccine recommendations since it was only recently introduced in the country. In our study, among 30 HCWs not immunized, 90% reported not knowing Tdap vaccine. Miller et al.23 found a lower percentage in United States: 39% of HCWs reported having never heard of the vaccine.
We have not actively accessed adverse events following immunization (AEFI) during our vaccination strategies, but one case of hypersensitivity reaction occurred during vaccination by mobile team at the workplace. The HCW was treated with intravenous corticosteroid and antihistamine, with full recovery (data not shown).
This study has limitations. First, we performed lectures only for physicians. Furthermore, vaccination of HCWs in their work sites was conducted in just one-day period in each clinic, given the shortage of human resources. These limitations may explain in part our low final vaccine coverage.
In conclusion, Tdap coverage among HCWs was low in our hospital, similarly to other reports in literature. Every healthcare facility should evaluate its vaccination coverage and promote continuous surveillance and strategies to raise Tdap uptake to prevent nosocomial pertussis outbreaks. Combination of different strategies is necessary, including increasing awareness on disease risk and vaccine effectiveness, safety and recommendations, and improving access to vaccination. Our data suggest that making access to vaccines easier, such as vaccination at workplace, at convenient times for the HCWs are critical. Importantly, mobile teams must be prepared to deal with immediate adverse events following immunization, particularly with hypersensitivity reactions. Finally, new approaches to reach adults, particularly the HCWs, to increase vaccines coverage among them are needed.
Conflicts of interestThe authors declare no conflicts of interest.