Herpesvirus reactivation is common after liver transplantation.
ObjectiveAnalyze the presence of cytomegalovirus (HCMV) and human herpesvirus-6 (HHV-6) DNA in liver donor biopsies, seeking to better understand issues involving human donor leukocyte antigens (HLA)-A, B and DR, as well as correlations with acute cellular rejection.
MethodsFifty-nine liver transplantation patients were investigated for the presence of HCMV and HHV-6 DNA in liver donor biopsies, using the Nested-PCR technique. The clinical donor information and HLA matches were obtained from the São Paulo State Transplant System. The recipients’ records regarding acute cellular rejection were studied.
ResultsSeven (11.8%) biopsies were positive for HCMV DNA and 29 (49%) were positive for HHV-6 DNA. In 14 donors with HLA-DR 15 nine had HHV-6 DNA positive liver biopsy with a tendency for significant association (p=0.09), 22 recipients developed acute cellular rejection and 9/22 were positive for HLA-DR 15 (p=0.03; χ2=4.51), which was statistically significant in univariate analysis and showed a tendency after multivariate analysis (p=0.08).
ConclusionHHV-6 DNA was prevalent in liver donors studied as well as HLA-DR 15. These findings suggest that patients with HLA-DR 15 in liver donor biopsies develop more rejection after liver transplantation.
In liver transplantation patients, cytomegalovirus (HCMV) and human herpesvirus-6 HHV-6 are the most common infections. These viruses undergo latency and reactivation episodes in the host. HCMV prevalence ranges from 20% to 60%. Among patients with active infections, 80% develop clinical manifestations of the disease; HHV-6 infections occur among in 14–82% of solid organ transplantations.1,2 HCMV infection may vary depending on baseline HCMV-specific immunity (donor and recipient seropositivity), the overall net state of immunosuppression. HCMV infection may be the result of reactivation or reinfection (in HCMV-seropositive recipients) or primary infection (in a HCMV-seronegative recipient who received an allograft from a HCMV-seropositive donor [D+/R−]).3
The role of human leukocyte antigen (HLA) between donor and recipient in organ transplantation has been widely studied and some authors suggest that HLA-A, B, or DR mismatch increases the incidence of HCMV hepatitis in both primary and secondary HCMV infections and is associated with increased graft failure. HHV-6 reactivation and infections after liver transplantation are asymptomatic, although the risk factors are not completely defined.4–6
The aim of the present study was to analyze the presence of HCMV and HHV-6 DNA in liver donor biopsies, seeking to better understand issues involving HLA-A, B, and DR donor, as well as associations with acute cellular rejection.
At the Clinical Hospital of the Sao Paulo State University in Campinas – Unicamp – in the period between January 2006 and December 2008, 59 orthotopic liver transplants were carried out at the Liver Transplant Unit. The patients were followed up and their donor liver biopsies were used in this study.
The liver biopsies were collected from the organ before transplantation at the bench (pre-transplant graft biopsy). This was an observational, analytic, longitudinal prospective cohort study.
Children and retransplantation patients were excluded from the study. A total of 59 patients enrolled met the following inclusion criteria: 1 – sufficient liver biopsy material for DNA virus analysis by the N-PCR method; 2 – clinical donors’ information available from the State Transplant System, São Paulo, Brazil.
The presence of HCMV and HHV-6 DNA N-PCR was investigated as well as their co-infection in liver donor biopsies. These analyses were performed in formalin-fixed paraffin-embedded material. Patients’ records were analyzed in the first six months post-transplant period to assess acute cellular rejection. HLA matches were obtained from the Sao Paulo transplant system.
All patients from this study had received prophylaxis for Herpes simplex infection and standard immunosuppressive therapy according to our protocol.7 All recipients had positive IgG for HCMV before transplantation and there was no recipient serology for HHV-6 before transplantation. All donors had positive serology for HCMV and no HHV-6 serology results.
Diagnosis and monitoring of graft acute cellular rejection were performed according to the Banff International Consensus.8 All acute rejection episodes were treated with methilprednisolone according to our protocol.
Viral DNA was extracted from liver biopsy specimens using the Qiagen Dneasy tissue kit (Uniscience, São Paulo, Brazil) according to the manufacturer's instructions with some modifications to achieve final elution volumes of 30μL.7
Five microliters of extracted DNA were used for the N-PCR for HCMV and HHV-6 using a mixture containing specific primers (HCMV primers; Invitrogen, São Paulo, Brazil), using a previously described technique9 with some modifications. Specific primers for HHV-6 (HHV-6 primers; Invitrogen) were applied with a technique previously described by Secchiero et al.10 with some modifications. The amplifications were performed in a Peltier Thermal Cycler (MJ Research, Waltham, MA, USA). The N-PCR products were analyzed under UV light after electrophoresis in agarose gel (Gibco-BRL Life Technology, Carlsbad, CA, USA) in tetramethylbenzidine buffer after staining with ethidium bromide. All primer sequences and PCR products were analyzed using the Genbank database before initiating the study. PCR using primers for beta-globin gene amplification, which were performed on samples to detect possible false-negative results, were not included in this study.7
Categorical variables were compared using Fisher's exact test and multiple regression analysis was performed using acute cellular rejection as the dependent variable by Statsoft 11.0 program (NY, USA, 2012). p<0.05 was considered statistically significant.
This study was approved by the Institutional Ethics Committee of the Faculty of Medical Sciences, UNICAMP (CEP no. 030/2006).
Fifty-nine liver donors were studied, 36 (61%) were men and 23 (39%) were women.
Thirty (51%) donors were of blood group O, 22 (37%) blood group A, five blood group B, and two group AB. The mean age was 32.2 years±13.0. Thirty-one (52%) donors died due to traumatic brain injury, 21 (35%) donors due to cerebrovascular accident (CVA) and seven donors had other causes of death.
Twenty-nine (49%) out of 59 donors studied had a positive serology for HHV-6 DNA and seven (11.8%) were for HCMV-DNA. Liver donor biopsies had a co-infection (HCMV and HHV-6) positivity rate of 10% (6/59).
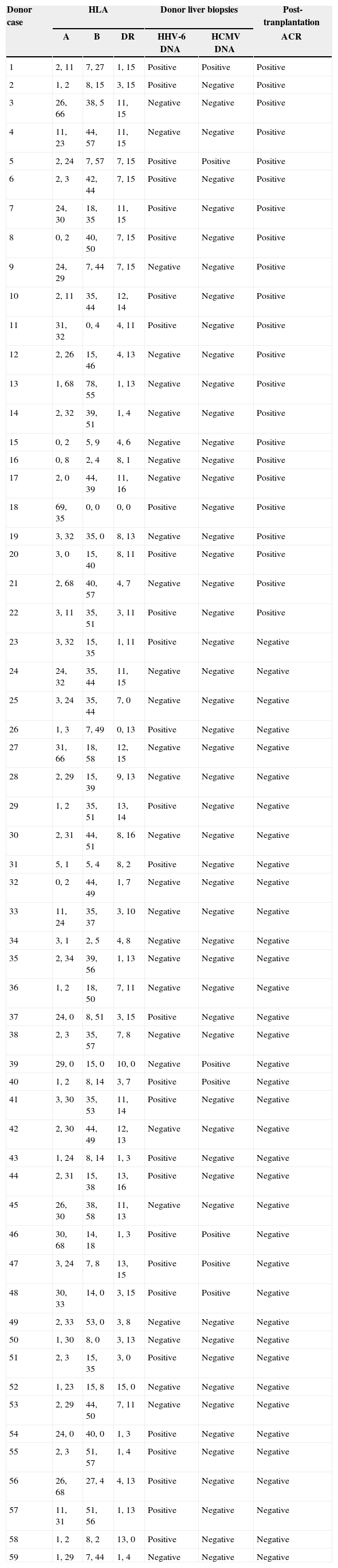
We also investigated HLA matches (A, B and DR locus) between HCMV-DNA and HHV-6-DNA. These data are described in Table 1. Of the 14 (23.7%) donors with HLA-DR15, nine (64%) were positive for HHV-6 DNA at liver biopsy with a tendency for significant association (p=0.09; Fisher's exact test). No association was found between CMV DNA positivity in liver biopsies and HLA-DR 15.
Donor HLA information association with HHV-6 and CMV DNA and acute cellular rejection in post-transplantation period.
| Donor case | HLA | Donor liver biopsies | Post-tranplantation | |||
|---|---|---|---|---|---|---|
| A | B | DR | HHV-6 DNA | HCMV DNA | ACR | |
| 1 | 2, 11 | 7, 27 | 1, 15 | Positive | Positive | Positive |
| 2 | 1, 2 | 8, 15 | 3, 15 | Positive | Negative | Positive |
| 3 | 26, 66 | 38, 5 | 11, 15 | Negative | Negative | Positive |
| 4 | 11, 23 | 44, 57 | 11, 15 | Negative | Negative | Positive |
| 5 | 2, 24 | 7, 57 | 7, 15 | Positive | Positive | Positive |
| 6 | 2, 3 | 42, 44 | 7, 15 | Positive | Negative | Positive |
| 7 | 24, 30 | 18, 35 | 11, 15 | Positive | Negative | Positive |
| 8 | 0, 2 | 40, 50 | 7, 15 | Positive | Negative | Positive |
| 9 | 24, 29 | 7, 44 | 7, 15 | Negative | Negative | Positive |
| 10 | 2, 11 | 35, 44 | 12, 14 | Positive | Negative | Positive |
| 11 | 31, 32 | 0, 4 | 4, 11 | Positive | Negative | Positive |
| 12 | 2, 26 | 15, 46 | 4, 13 | Negative | Negative | Positive |
| 13 | 1, 68 | 78, 55 | 1, 13 | Negative | Negative | Positive |
| 14 | 2, 32 | 39, 51 | 1, 4 | Negative | Negative | Positive |
| 15 | 0, 2 | 5, 9 | 4, 6 | Negative | Negative | Positive |
| 16 | 0, 8 | 2, 4 | 8, 1 | Negative | Negative | Positive |
| 17 | 2, 0 | 44, 39 | 11, 16 | Negative | Negative | Positive |
| 18 | 69, 35 | 0, 0 | 0, 0 | Positive | Negative | Positive |
| 19 | 3, 32 | 35, 0 | 8, 13 | Negative | Negative | Positive |
| 20 | 3, 0 | 15, 40 | 8, 11 | Positive | Negative | Positive |
| 21 | 2, 68 | 40, 57 | 4, 7 | Negative | Negative | Positive |
| 22 | 3, 11 | 35, 51 | 3, 11 | Positive | Negative | Positive |
| 23 | 3, 32 | 15, 35 | 1, 11 | Positive | Negative | Negative |
| 24 | 24, 32 | 35, 44 | 11, 15 | Negative | Negative | Negative |
| 25 | 3, 24 | 35, 44 | 7, 0 | Negative | Negative | Negative |
| 26 | 1, 3 | 7, 49 | 0, 13 | Positive | Negative | Negative |
| 27 | 31, 66 | 18, 58 | 12, 15 | Negative | Negative | Negative |
| 28 | 2, 29 | 15, 39 | 9, 13 | Negative | Negative | Negative |
| 29 | 1, 2 | 35, 51 | 13, 14 | Positive | Negative | Negative |
| 30 | 2, 31 | 44, 51 | 8, 16 | Negative | Negative | Negative |
| 31 | 5, 1 | 5, 4 | 8, 2 | Positive | Negative | Negative |
| 32 | 0, 2 | 44, 49 | 1, 7 | Negative | Negative | Negative |
| 33 | 11, 24 | 35, 37 | 3, 10 | Negative | Negative | Negative |
| 34 | 3, 1 | 2, 5 | 4, 8 | Negative | Negative | Negative |
| 35 | 2, 34 | 39, 56 | 1, 13 | Negative | Negative | Negative |
| 36 | 1, 2 | 18, 50 | 7, 11 | Negative | Negative | Negative |
| 37 | 24, 0 | 8, 51 | 3, 15 | Positive | Negative | Negative |
| 38 | 2, 3 | 35, 57 | 7, 8 | Negative | Negative | Negative |
| 39 | 29, 0 | 15, 0 | 10, 0 | Negative | Positive | Negative |
| 40 | 1, 2 | 8, 14 | 3, 7 | Positive | Positive | Negative |
| 41 | 3, 30 | 35, 53 | 11, 14 | Positive | Negative | Negative |
| 42 | 2, 30 | 44, 49 | 12, 13 | Negative | Negative | Negative |
| 43 | 1, 24 | 8, 14 | 1, 3 | Positive | Negative | Negative |
| 44 | 2, 31 | 15, 38 | 13, 16 | Positive | Negative | Negative |
| 45 | 26, 30 | 38, 58 | 11, 13 | Negative | Negative | Negative |
| 46 | 30, 68 | 14, 18 | 1, 3 | Positive | Positive | Negative |
| 47 | 3, 24 | 7, 8 | 13, 15 | Positive | Positive | Negative |
| 48 | 30, 33 | 14, 0 | 3, 15 | Positive | Positive | Negative |
| 49 | 2, 33 | 53, 0 | 3, 8 | Negative | Negative | Negative |
| 50 | 1, 30 | 8, 0 | 3, 13 | Negative | Negative | Negative |
| 51 | 2, 3 | 15, 35 | 3, 0 | Positive | Negative | Negative |
| 52 | 1, 23 | 15, 8 | 15, 0 | Negative | Negative | Negative |
| 53 | 2, 29 | 44, 50 | 7, 11 | Negative | Negative | Negative |
| 54 | 24, 0 | 40, 0 | 1, 3 | Positive | Negative | Negative |
| 55 | 2, 3 | 51, 57 | 1, 4 | Positive | Negative | Negative |
| 56 | 26, 68 | 27, 4 | 4, 13 | Positive | Negative | Negative |
| 57 | 11, 31 | 51, 56 | 1, 13 | Positive | Negative | Negative |
| 58 | 1, 2 | 8, 2 | 13, 0 | Positive | Negative | Negative |
| 59 | 1, 29 | 7, 44 | 1, 4 | Negative | Negative | Negative |
HLA, human leukocyte antigens; HCMV, cytomegalovirus; HHV-6, human herpesvirus-6; ACR, acute cellular rejection.
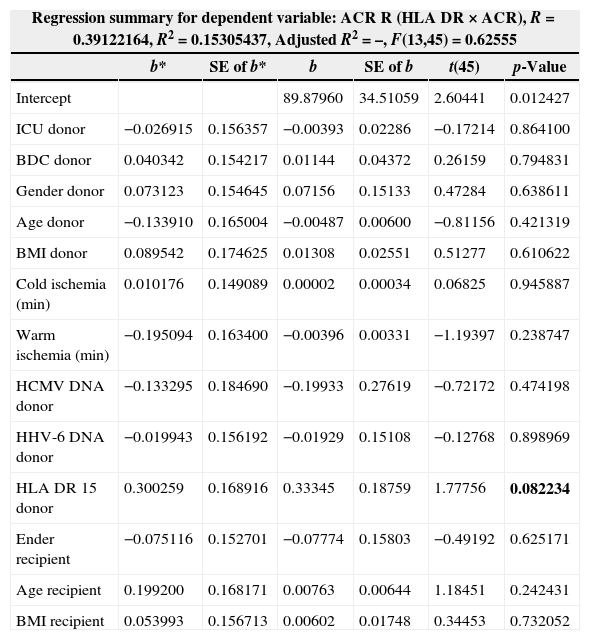
After liver transplantation, 22 (37%) recipients developed acute cellular rejection and 41% (9/22) had HLA-DR15 (p=0.03; χ2=4.51; Fisher's exact test). Moreover, in multivariate analysis presence of DR15 had a tendency to be associated with acute cellular rejection after transplantation (Table 2). Likewise, HLA DR15 was associated with HHV-6 positivity in donor biopsies.
Multivariate regression analysis and clinical variables using ACR as dependent variable.
| Regression summary for dependent variable: ACR R (HLA DR×ACR), R=0.39122164, R2=0.15305437, Adjusted R2=–, F(13,45)=0.62555 | ||||||
|---|---|---|---|---|---|---|
| b* | SE of b* | b | SE of b | t(45) | p-Value | |
| Intercept | 89.87960 | 34.51059 | 2.60441 | 0.012427 | ||
| ICU donor | −0.026915 | 0.156357 | −0.00393 | 0.02286 | −0.17214 | 0.864100 |
| BDC donor | 0.040342 | 0.154217 | 0.01144 | 0.04372 | 0.26159 | 0.794831 |
| Gender donor | 0.073123 | 0.154645 | 0.07156 | 0.15133 | 0.47284 | 0.638611 |
| Age donor | −0.133910 | 0.165004 | −0.00487 | 0.00600 | −0.81156 | 0.421319 |
| BMI donor | 0.089542 | 0.174625 | 0.01308 | 0.02551 | 0.51277 | 0.610622 |
| Cold ischemia (min) | 0.010176 | 0.149089 | 0.00002 | 0.00034 | 0.06825 | 0.945887 |
| Warm ischemia (min) | −0.195094 | 0.163400 | −0.00396 | 0.00331 | −1.19397 | 0.238747 |
| HCMV DNA donor | −0.133295 | 0.184690 | −0.19933 | 0.27619 | −0.72172 | 0.474198 |
| HHV-6 DNA donor | −0.019943 | 0.156192 | −0.01929 | 0.15108 | −0.12768 | 0.898969 |
| HLA DR 15 donor | 0.300259 | 0.168916 | 0.33345 | 0.18759 | 1.77756 | 0.082234 |
| Ender recipient | −0.075116 | 0.152701 | −0.07774 | 0.15803 | −0.49192 | 0.625171 |
| Age recipient | 0.199200 | 0.168171 | 0.00763 | 0.00644 | 1.18451 | 0.242431 |
| BMI recipient | 0.053993 | 0.156713 | 0.00602 | 0.01748 | 0.34453 | 0.732052 |
Abbreviations: ACR, acute cellular rejection; ICU, internal care unit; BDC, brain death cause; HLA, human leukocyte antigens; HCMV, cytomegalovirus; HHV-6, human herpesvirus-6; BMI, body mass index; SE, standard error; b, beta.
The results of the present study indicate that HHV-6 DNA and HCMV DNA were commonly detected in donor liver transplantation at the Liver Transplant Unit – Unicamp, as shown in other studies we have previously carried out.11 HHV-6 and HCMV in patients are common after liver transplantation and the interaction of these viruses can increase their pathogenic effects.12–14
In our study, HHV-6 DNA was observed in 49% and HCMV DNA in 11.8% of donor liver biopsies. We could find no published reports to confirm these data but it is known that these viruses can have an incidence of over 80% (serologic status) in the human population.15,16 This is an important fact because herpesviruses can establish a latent infection for the lifetime of the host.17 A recent study identified high intrahepatic HHV-6 viral load, suggesting that HHV-6 reactivation in the liver graft is of clinical relevance.18
In our results, of 23.7% (14/59) HLA-DR15 donors, nine 9 (64%) had positive HHV-6 DNA at liver biopsy with a tendency to have significant association. No association was found between CMV DNA positivity in liver biopsies and HLA-DR15 presence.
Some studies have suggested that HLA compatibility can have clinical significance after liver transplantation.4,5 Manez et al. suggest that an HLA-DR mismatch between donor and recipient increases the incidence of HCMV hepatitis and infections.4 Another study examined the incidence of HCMV viremia after liver transplantation with the HLA matching influence, and found no association.19
Some patients in this study developed graft rejection associated with HLA-DR15. An a recent study we showed that 51% of the recipients developed graft rejection.11 Acute or chronic rejection remains the most common reason for graft failure, especially for patients who have HLA mismatching.6 The role of HLA matching between donor and recipient in organ transplant rejection has been pointed out in some studies and a degree of HLA mismatching could be associated with increased graft failure.6,20 Menez et al. showed that HLA-DR mismatching may accelerate chronic rejection of liver transplants.4
In summary HHV-6 DNA was prevalent in liver donors studied as well as HLA-DR15. These findings suggest that detection of HLA-DR15 in liver donor biopsies developed more rejection after liver transplantation. However, further studies are necessary to clarify these data, especially HHV-6 infection in donor samples together with HLA mismatches.
Conflicts of interestThe authors declare no conflicts of interest.