Cardiovascular disease in the context of human immunodeficiency virus infection has become a major clinical concern in recent years. In the current report we assess hospitalizations due to cardiovascular disease in human immunodeficiency virus patients in a Social Security reference hospital in Peru.
MethodsA retrospective study was carried out between January 1996 and December 2012 in a General Hospital in Lima, Peru.
ResultsWe included 26 patients hospitalized due to cardiovascular disease. Mean age was 46.3 years (SD 12.5), predominantly male (57.7%). Ten patients (38.4%) were in Acquired Immunodeficiency Syndrome stages. Seventeen (65.4%) received high-active-antiretroviral therapy. Eleven (42.3%) had cardiac involvement and 15 (57.7%) had non-cardiac vascular involvement. The most frequent causes of cardiac involvement were pericardial effusion and myocardial infarction. On the other hand, deep vein thrombosis and stroke were the most frequent for non-cardiac vascular involvement.
ConclusionsCardiovascular disease is an important cause of hospitalization in Peruvian human immunodeficiency virus patients, with differences between immunosuppression stages. Further studies analyzing associated factors are warranted.
Human immunodeficiency virus (HIV) infection has been characterized by significant immunosuppression states that predispose patients to opportunistic infectious and neoplasias, as well as progressive dysfunction of organs and systems.1 Since 1981, HIV infection, and particularly the Acquired Immunodeficiency Syndrome (AIDS), has evolved drastically from an acute lethal condition, with no therapeutic options, to a chronic disease with multiple available therapeutic regimens.2 Unfortunately, AIDS epidemic affects primarily young adults, including a percentage of skilled educated persons causing high economic impact. Furthermore, it is still associated with stigma that could probably limit the response to this epidemic.3 In Latin-America there are important differences between countries. According to data from ONUSIDA and CELADE, in 2010 there were 75,000 HIV-infected patients in Peru with a prevalence of 2.5 per 1000 inhabitants, being sexual intercourse the most important route of transmission (97%).4
Highly active antiretroviral therapy (HAART) significantly reduced morbidity and mortality related to AIDS-defining opportunistic diseases (ODs).4 Since the introduction of dideoxynucleoside reverse transcriptase inhibitors (NRTIs) in 1985 and after the approval of the first protease inhibitor in 1995, the availability of new fixed-dose combinations regimens of new antiretroviral drugs, evolved faster in the developed world. Unfortunately, this is not the situation in low- and middle-income countries, especially in the rural setting, where HIV now is common.5 The successful role of HAART has extended life expectancy and enhanced the overall well-being of HIV-infected individuals. Moreover, recent reports demonstrated that HAART could be useful strategy in prevention, as well as in treatment, point out the importance of drug adherence.4,5 In Peru, EsSalud, a major social security health provider, incorporated HAART in 2001 with increasing coverage, as the medical and patient communities readily accepted it.4
However, there are increased concerns regarding HAART-mediated metabolic derangements and its potential risk for cardiovascular diseases (CVD) in the long term,1,3,5 especially when certain classes of antiretroviral drugs, such as the protease inhibitors (PIs) are strongly implicated in this process.6 CVD in HIV infection may result from cardiac involvement upon presentation of ODs in the presence of advanced immunosuppression, be a consequence of HIV-induced immune activation or derive from antiretroviral therapy-associated dyslipidemia and insulin resistance.7 Besides that, such consequences have not been particularly addressed in Latin American countries, including Peru.1–7
CVD in patients with HIV infection, must be diagnosed and treated, because there is growing incidence, due to factors associated with the infection or with the use of some therapies.6 According to the Joint United Nations Program on HIV and AIDS (UNAIDS) 2013 report, it has been estimated that 35.3 million were infected all over the world in 2012 (32.2 million–38.8 million). However, the annual incidence of new cases are decreasing as a consequence of HAART use.8 Nonetheless, if on one hand new complex therapeutic regimens have favorably impacted life expectancy, on the other hand some clinical situations like CVD or adverse events have become very relevant.6,9 Investigations assessing these negative consequences of HAART should be conducted in settings like Peru, where there have no previous studies.10–15
Therefore, the aim our study was to describe the CVD complications as a cause of hospitalization in HIV-infected patients, in every stage of disease, in a General Hospital of Social Security in Lima, Peru.
We carried out a retrospective observational study (case series) at the Edgardo Rebaglati Martins Hospital, a reference hospital from Peruvian Social Security (EsSalud), with 1500 beds, at Lima, Peru. This report corresponds to the period between January 1996 and December 2012.
Every hospitalization at the Infectious Diseases Unit during the study period was reviewed, looking for the diagnosis of HIV infection that ought to be described in the diagnosis list filled in at hospital admission and discharge. At discharge, diagnosis of “acute pericarditis”, “other diseases of pericardium”, “unstable angina”, “acute myocardial infarction”, “myocarditis”, “acute and subacute endocarditis”, “heart failure”, “cerebral infarction”, “intracerebral hemorrhage”, “thrombophlebitis”, “pulmonary embolism”, and “primary pulmonary hypertension”, according to ICD-10 classification, were reviewed.
Cardiovascular risk factors were defined as follows: arterial hypertension according to recommendations of the Seventh Joint National Committee or if the patient reported to be on hypertensive treatment; diabetes was defined if the patient had glucose level of 126mg/dL or greater in two separate occasions, or if the patient was on treatment for this condition. Dyslipidemia was considered if the patient had total cholesterol of 200mg/dL or greater, or were receiving hypocholesterolemic drugs. Obesity was considered when in patients with a body mass index of 30 or greater. Finally, a patient classified as smoker if he smoked any number of cigarettes at the time of hospital admission or had quitted smoking less than a year before.
Data of clinical records of the eligible patients were abstracted using a form built for this study. Analysis was performed using the Statistical Package for Social Science (SPSS) version 21.0 (IBM Corporation 1994, 2014, USA). At descriptive level numeric variables were presented as means and standard deviations (SD) if they had normal distribution or with medians and interquartile ranges (IQR) if they had not. Categorical variables are showed as absolute frequencies and percentages.
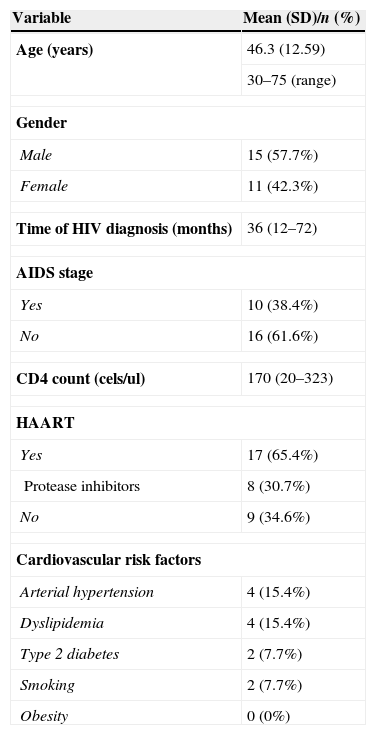
We included 26 hospitalized HIV-infected patients with CVD in study period. No patient had more than one hospitalization for the same reason. Mean age was 46.3 years (SD 12.5), and were predominantly male (57.7%). Ten patients (38.4%) fulfilled the definition of AIDS. Out of the 17 (65.4%) patients who had received HAART, eight had received protease inhibitors. The overall median time of HAART use was 48 months (IQR 72), and of HAART including protease inhibitors was 72 months (IQR 90).
Prevalence of cardiovascular risk factors was low, with 15.4% with arterial hypertension and dyslipidemia, and type 2 diabetes or smoking in 7.7% (Table 1).
Demographic and clinical variables of HIV-infected patients with cardiovascular diseases at Edgardo Rebagliati Martins Hospital, Lima, Peru, 1996–2012.
| Variable | Mean (SD)/n (%) |
|---|---|
| Age (years) | 46.3 (12.59) |
| 30–75 (range) | |
| Gender | |
| Male | 15 (57.7%) |
| Female | 11 (42.3%) |
| Time of HIV diagnosis (months) | 36 (12–72) |
| AIDS stage | |
| Yes | 10 (38.4%) |
| No | 16 (61.6%) |
| CD4 count (cels/ul) | 170 (20–323) |
| HAART | |
| Yes | 17 (65.4%) |
| Protease inhibitors | 8 (30.7%) |
| No | 9 (34.6%) |
| Cardiovascular risk factors | |
| Arterial hypertension | 4 (15.4%) |
| Dyslipidemia | 4 (15.4%) |
| Type 2 diabetes | 2 (7.7%) |
| Smoking | 2 (7.7%) |
| Obesity | 0 (0%) |
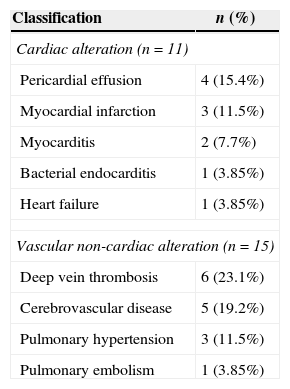
Eleven patients (42.3%) had some type of cardiac alteration and 15 (57.7%) had some type of vascular non-cardiac problem. The most frequently cardiac alterations were pericardial effusion (15.4%) and myocardial infarction (11.5%); among vascular non-cardiac alterations prevailed deep vein thrombosis (23.1%) and cerebrovascular disease (19.2%) (Table 2).
Frequency of cardiovascular alterations of HIV-infected patients with cardiovascular disease at Edgardo Rebagliati Martins Hospital, Lima, Peru, 1996–2012.
| Classification | n (%) |
|---|---|
| Cardiac alteration (n=11) | |
| Pericardial effusion | 4 (15.4%) |
| Myocardial infarction | 3 (11.5%) |
| Myocarditis | 2 (7.7%) |
| Bacterial endocarditis | 1 (3.85%) |
| Heart failure | 1 (3.85%) |
| Vascular non-cardiac alteration (n=15) | |
| Deep vein thrombosis | 6 (23.1%) |
| Cerebrovascular disease | 5 (19.2%) |
| Pulmonary hypertension | 3 (11.5%) |
| Pulmonary embolism | 1 (3.85%) |
Cardiac involvement in HIV-infected patients with AIDS was first described in 1983 by Autran who reported myocardial Kaposi sarcoma at autopsy. After that, there have been an increased number of reports of cardiac involvement in AIDS patients ranging between 28% and 73%. Moreover, in autopsy reports of HIV-infected patients, the findings suggest that cardiac involvement is rather common, possibly affecting more than 73% of patients.16,17
However, with the increase of life expectancy of the HIV-infected population, the incidence of age-related diseases, such as CVD in older adults, have also increased. Such increment in CVD has been related to aging, where some cardiovascular risk factors like high blood pressure and diabetes, as well as to the use of antiretroviral therapies, whose effect could be different depending on the therapeutic class and the individual effects of every drug.17–20
Prevalence of these CVD in HIV-infected patients varies from country of origin (developing or developed regions) and according to the use of HAART and the type of therapy (including protease inhibitors or not). On the other hand, vascular involvement associated with HIV infection or its treatment could be cardiac or non-cardiac.17–20
In Peru, there are some publications about the cardiac involvement of HIV-infected patients. In a study of 164 ambulatory patients from Cayetano Heredia (Ministry of Health) and Guillermo Almenara (Social Security, EsSalud), evaluated during 2001 and 2002, using echocardiography, the prevalences of CVD complications were: pericardial effusion 9.75%, systolic dysfunction 1.82%, diastolic dysfunction 26.82%, restrictive cardiomyopathy 0.60%, and pulmonary hypertension 2.43%.16 These results suggest that CVD could be present in patients without cardiovascular symptoms, because none of them had a previous positive cardiovascular evaluation.
In 2006, we evaluated a group of ambulatory patients with HIV infection who were on HAART. Arterial hypertension was present in 3.26%, type 2 Diabetes in 1.81%, dyslipidemia in 34.05%, smoking in 3.96% and obesity in 4.71%.
Of this population, 4.16% who received protease inhibitors had a high cardiovascular risk score according with Framingham in comparison with patients who did not receive protease inhibitors, which had a moderate cardiovascular risk score in 12.03% and a high cardiovascular risk score in 0.92%.21
In the present study, we described forms of cardiac and non-cardiac vascular alterations, as causes for hospitalization at Rebagliati hospital, a national reference hospital in the country. Cardiac causes were pericardial effusion, myocardial infarction, myocarditis, bacterial endocarditis and heart failure. None of these patients had cardiovascular risk factors or were on antiretroviral therapy at the time of complication. Pericardial effusion was the most frequent cardiovascular manifestation (4 cases). Study of the pericardial fluid was not performed according with the hospital protocols.
Pericardial effusion in patients with HIV infection could be related with infections by opportunistic agents or malignant neoplasms, but more frequently the etiology is unknown. Additionally, pericardial effusion could spontaneously resolve in more than 42%,7–9,16–18 considering that AIDS patients with pericardial effusion have an annual incidence of cardiac tamponade of 9%, and that 1% of patients with AIDS, annually develop this medical condition.16
We identified three cases of myocardial infarction, being with ST elevation in two cases and with no ST elevation in one case. ST elevation myocardial infarction had more than two cardiovascular risk factors (dyslipidemia and smoking; hypertension, type 2 diabetes, dyslipidemia and smoking) and did not receive fibrinolytics or coronary angioplasty for the acute phase, despite having formal indications to receive them. One patient with ST elevation myocardial infarction died from sudden cardiac death three months after discharge. Moreover, there was no case of myocardial infarction associated with pericardial effusion.
The relationship between viral infections and coronary artery disease has not yet been fully established. Potential mechanisms by which HIV virus could damage coronary arteries include the activation of cytokines and adhesion molecules, and some alterations of class I tissue histocompatibility molecules in the surface of smooth muscle cells.11 However, in the last decades, there were reported cases of acute coronary syndromes (unstable angina or myocardial infarction) in patients with HIV infection who were on antiretroviral therapy. Patients with additional risk factors, like arterial hypertension, type 2 diabetes, smoking, or hyperhomocysteinemia could have an increased risk to develop acute coronary syndromes or cerebrovascular disease, because of accelerated atherosclerosis.16–19
We found two cases of myocarditis, one case of heart failure, and another case of bacterial endocarditis. One case of myocarditis was diagnosed in the debut of HIV infection and the other case was a young woman with less than two years of HIV diagnosis. The case of heart failure was diagnosed in a patient with previous mitral valve involvement, and the case of bacterial endocarditis was a patient without previous cardiac disease, who received empirical antibiotic therapy with good response.
The rate of bacterial endocarditis in patients with HIV infection is similar to other groups of risk, like IV drug users. The prevalence varies from 6.3% to 34% in patients with HIV infection, who are also IV drug users.7,8 It is possible to find cases of non-bacterial thrombotic endocarditis (marantic endocarditis), and this is present in 3–5% of AIDS patients, mainly in those with wasting syndrome.18,19
Cardiac involvement in HIV-infected patients was more frequently present in AIDS patients. It has been published that pericardial effusion and myocarditis could be present in later stages of infection. On the other hand, myocardial infarction, always severe, could be present in every stage of disease.1,2,18–20
In our report, we described some cases of vascular non-cardiac disease, like sic cases of deep vein thrombosis, five cases of cerebrovascular disease, three cases of pulmonary hypertension, and one case of pulmonary embolism. All of the deep vein thrombosis cases received antiretroviral therapy, and three of them received protease inhibitor agents. We know that some antiretroviral agents, like protease inhibitors induce insulin resistance, and then an increase of sympathetical activity with sodium retention and subsequent arterial hypertension. Other reports indicated that elevated blood pressure could be related to lipodistrophy and other metabolic disorders, especially in patients with hypertriglicerydemia. Moreover, patients with HIV infection that develop fat distribution, could have coagulation disorders like increased levels of fibrinogen, D-dimer, inhibitor of plasminogen activator, and decreased levels of S protein. These abnormalities had been associated with both arterial and venous thrombosis.10–15
All cases with cerebrovascular disease were ischemic and affected individuals below 60 years of age (mean age 44.8 years). Four of them, were on antiretroviral therapy (two on protease inhibitors). Only one of them had type 2 diabetes as a cardiovascular risk factor.
Brain infarction or hemorrhage as manifestations of HIV infection has been less studied. More recent series of patients, described a greater proportion of cases with brain infarction (90–95% of cases) compared to hemorrhage (5–10% of cases). In brain infarctions, the cause is found in most patients, and disorders of coagulations are common. Deficiency in S protein, increased levels of IgG anti-phospholipid antibodies, and anti-cardiolipin antibodies have been described. Most of the patients in this series had lower than 500 CD4 cells/UL.10–15
Three cases had pulmonary hypertension not associated with cardiac or pulmonary disease. One case received antiretroviral therapy without protease inhibitors. The incidence of pulmonary hypertension associated with HIV infection is approximately 1/200, a much greater incidence than in the overall population, which is 1/200,000. This clinical entity had been related with the presence of pulmonary infections, IV drug abuse, factor VIII transfusion in hemophilic patients, venous thromboembolism, heart failure, and the presence of HLA-D26 and HLA-DR52.10–15
Vascular non-cardiac alterations in our case-series was more frequently observed than cardiac alterations, and were associated with early stages of infection. In this report, we evaluated vascular cardiac or non-cardiac atherosclerotic complications, well defined and presented in clinical studies as cardiovascular endpoints. However, it is possible to detect subclinical atherosclerosis measuring carotid intima-media thickening (CIMT) or endothelial function using flow mediated brachial artery vasodilation.15
Compared to the pre-HAART era the number of deaths has declined all over the world after HAART use. This had been confirmed by some epidemiological studies, like the analysis of some centers controlled by US Department of Defense. Then, 987 deaths in the pre-HAART era were registered, compared to 159 deaths in early-HAART, and 78 deaths in well-established HAART era (p<0.01). On the other hand, there has been an increase of deaths not related to HIV infection by itself, and an increase in mortality due to cardiac involvement (22% vs. 8%). In this case registry in particular, cases between 1990 and 2003 were included and HAART was initiated in 1997.14
In our study, there were three cases (11.53%) of deaths for CVD. One patient died due to a massive cerebrovascular disease in the territory of middle cerebral artery, another due to a sudden cardiac as a complication of myocardial infarction, and the third patient due to pericardial effusion in a severely immunosuppressed case.
In the INSERM registry in France, the causes of death in patients with HIV infection in 2005 were compared to a previous evaluation performed in 2000. The percentage of death related to AIDS declined from 47% to 36%. However, there was an increase of three causes of death: neoplastic diseases, liver diseases, and CVD.13
The number of hospitalizations in persons living with HIV in the HAART era is not well known. However, the hospitalizations between 2001 and 2008 were evaluated in 11,645 individuals who received attention in US clinics. In this study, the hospitalizations for AIDS-related diseases declined from 6.7 to 2.7 per 100-persons/year, and the AIDS-defining infectious diseases, psychiatric, or hepatic/CVD were stable or diminished.11
Some demographic factors had been studied in 91,343 admissions in US between 2000 and 2004. In this report, the mean age was between 41 and 44 years and the number of diagnosis increased from 6 (2000) to 7.4 (2004), and the total number of hospitalizations reduced by 39%.12
In Latin America, after a careful review in bibliographic databases (Index Medicus/Medline, Scopus, Science Citation Index and SciELO), we did not find studies related to cardiovascular causes of hospitalization in HIV patients. Therefore, our study, in spite of being descriptive and conducted in a single center, is relevant given the fact it describes for the first time, cardiovascular events as hospitalization causes in HIV patients.
It has been estimated that the number of cardiovascular or metabolic complications in patients infected with HIV will progressively increase, as result of the increase in life-expectancy. For 2015, it is estimated that more than half of the infected patients will be over 50 years of age in the US, and all over the world there will be increased number of cases with access to antiretroviral therapy.10–15
Finally, in our study, we found a group of patients hospitalized due to CVD, with an approximate frequency of one or two cases per year. We firstly described a group of vascular cardiac and non-cardiac diseases that prompted hospitalization HIV-infected patients in different stages of the disease. According to our data, the presence of more advanced immunosuppression could be associated with higher probability of cardiac alterations. Further analytic studies in our country and at regional settings are warranted.
FundingSelf-funded.
Conflict of interestThe authors declare no conflicts of interest.